CGM Dose Adjustment Calculator
How to Use This Calculator
Follow these steps:
- Select your current glucose level in mg/dL
- Choose the trend arrow you're seeing
- Enter your correction factor (e.g., 1:50)
- Input carbohydrates in your meal
- Toggle pediatric mode if applicable
Trend arrows explained:
Adjust your insulin dose based on your CGM trend data.
Enter values above to see your personalized adjustment.
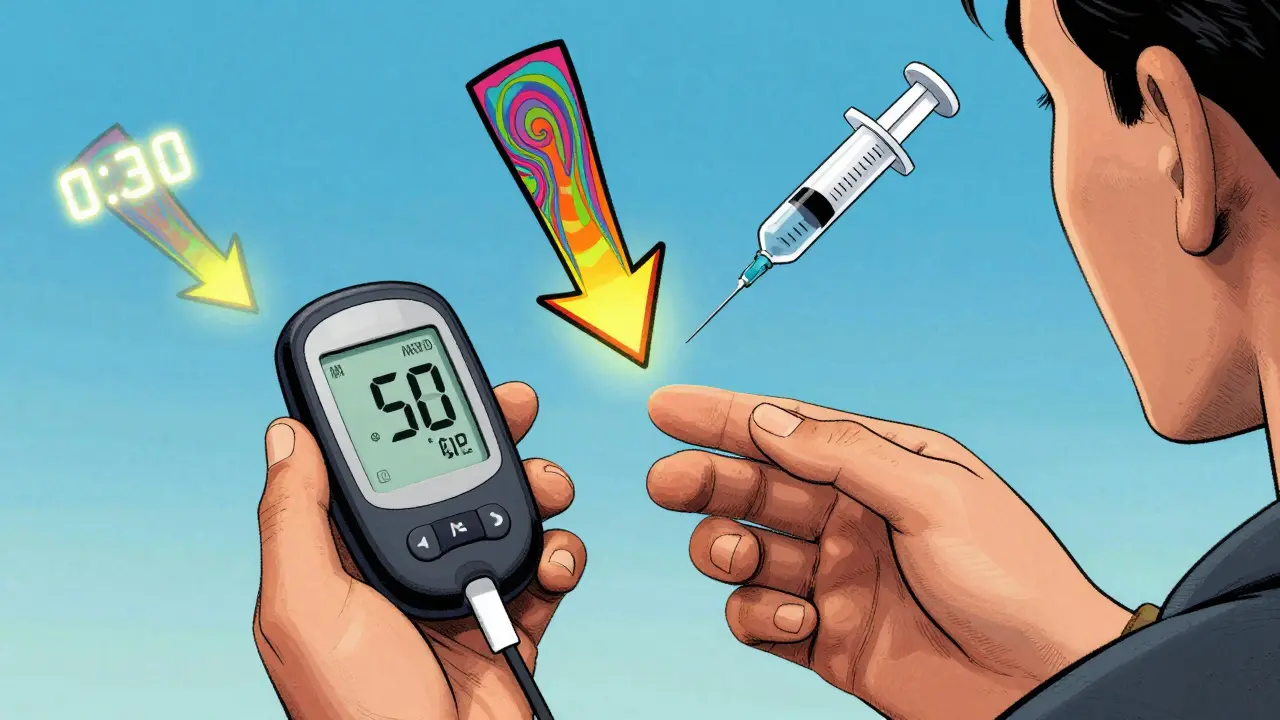
When you’re managing diabetes with insulin, the biggest fear isn’t just high blood sugar-it’s the sudden crash. A CGM doesn’t just show you your number. It tells you where it’s going next. And that changes everything.
Most people still adjust insulin based on a single number from a fingerstick. But that’s like driving with your eyes closed most of the time. You only open them long enough to check the speedometer. A CGM gives you the whole windshield. The trend arrows-those little up and down symbols on your screen-are your early warning system. They don’t just alert you to a problem. They tell you how to fix it before it happens.
What the Arrows Really Mean
Your CGM doesn’t just spit out a glucose reading. It calculates the direction and speed of change over the last 15 to 30 minutes. That’s why you see different arrows: single-up, double-up, flat, single-down, double-down. Each one means something specific.
Double-down? Your blood sugar is falling fast-maybe 3 to 4 mg/dL per minute. That’s not a gentle dip. That’s a freefall. If you’re about to eat and you see this, your usual bolus could send you into a low. Single-up? You’re rising slowly, maybe 1 to 2 mg/dL per minute. That’s a nudge, not a sprint. And flat? It’s steady. No change. No adjustment needed.
These aren’t guesses. They’re based on real-time data from your sensor. And they’re backed by science. The Endocrine Society published clear guidelines in 2017 showing exactly how much insulin to add or subtract based on these arrows. It’s not about percentages. It’s about units. Simple. Direct. Actionable.
How to Adjust Insulin Based on Trends
Let’s say your correction factor is 1:50. That means one unit of insulin lowers your blood sugar by 50 mg/dL. That’s common for adults. Now, if your glucose is 180 mg/dL and you’re seeing a double-up arrow before a meal, your usual dose might not be enough. The guidelines say: add 1.2 units to your meal bolus. Why? Because your body is already racing toward 200 or 220. You’re not just correcting the current number-you’re stopping the trend.
On the flip side, if your glucose is 170 mg/dL and you’re seeing a double-down arrow, you might not need any correction at all. In fact, you should reduce your usual dose by 1.2 units. Why risk dropping to 80 when you’re already falling fast? This isn’t counterintuitive-it’s preventive.
Pediatric dosing is different. Kids are more sensitive. For the same trend arrows and correction factor, the adjustment is smaller: +1.0, +0.6, 0, -0.6, -1.0 units. That’s because their insulin action is faster and their bodies respond more sharply. Parents who use this method report fewer nighttime lows and less panic.
Why This Beats Fingersticks
Traditional blood glucose meters give you a snapshot. CGMs give you a movie. A 2017 study in Diabetes Technology & Therapeutics showed people using trend arrows had 28% fewer low blood sugar events and spent 17% more time in target range. That’s not a small gain. That’s life-changing.
Think about it: you see your glucose is 150. You take your usual correction. But if it’s falling fast, you just pushed it lower. You didn’t know that. With a CGM, you see the double-down arrow. You hold off. You wait. You eat a snack. You avoid the crash.
And it works the other way too. You see a double-up before breakfast. You’ve been 120 all morning. Your usual dose would be fine for 120. But if it’s shooting up, you’re going to hit 250 by noon. Add the extra units. You stay steady.

When Not to Adjust
These rules aren’t magic. They don’t work if you ignore context.
Don’t adjust if your sensor is new. First 24 hours? Skip it. The sensor is still calibrating. Don’t adjust if you’ve had insulin in the last 2 to 3 hours. That’s insulin-on-board (IOB). If you’re seeing a double-down arrow but you took a correction 90 minutes ago, you’re not falling because of food-you’re falling because your last dose is still working. Adding more insulin now? That’s how you get a 45 mg/dL low.
And don’t adjust for a single arrow if you’re sick, exercising, or drinking alcohol. Those things change how your body uses insulin. Trend arrows are great for routine days-not chaos days.
Common Mistakes and How to Avoid Them
People make the same errors over and over.
Mistake 1: "I saw a double-up, so I doubled my insulin." That’s not how it works. You add 1.2 units-not double. If your usual dose is 4 units, you go to 5.2. Not 8.
Mistake 2: "I saw a double-down, so I skipped my insulin completely." That’s risky if you’re eating. You still need carbs covered. Just reduce the dose, don’t zero it.
Mistake 3: "I don’t trust the arrows." But you trust your fingerstick? A CGM gives you 288 readings a day. A meter gives you 4. Which one gives you more data to make smarter choices?
The biggest barrier? Lack of education. A 2021 survey found 39% of users didn’t use trend arrows because their provider never taught them how. That’s unacceptable. This isn’t optional anymore. It’s part of standard care.

It’s Not Just for Insulin
Most people think this only applies to insulin. But newer guidelines from the ADA and EASD in 2024 now include non-insulin drugs. Take SGLT2 inhibitors-meds like dapagliflozin or empagliflozin. They help lower glucose by making your kidneys dump sugar. But if your CGM shows persistent euglycemic ketosis-glucose under 180 but ketones above 0.6 mmol/L-you’re at risk for diabetic ketoacidosis (DKA), even if your sugar looks fine.
In those cases, your provider might tell you to reduce the SGLT2 inhibitor dose. Not because your sugar is high-but because your body is burning fat too fast. CGM trend data, paired with ketone readings, gives you the full picture.
What’s Next? AI and Automation
The next leap isn’t just arrows-it’s prediction. The FDA cleared a new app in 2023 called DAFNE+ that uses Dexcom G6 data to auto-calculate adjustments. It takes your current glucose, trend arrow, IOB, carbs, and insulin sensitivity-and spits out the right dose. Clinical trials showed a 62% drop in dosing errors.
And it’s getting smarter. Verily’s Onduo platform used machine learning to predict glucose changes 45 minutes ahead-not just 15. In a 2022 pilot, users had 38% fewer lows. This isn’t sci-fi. It’s here.
But here’s the catch: no app replaces understanding. You still need to know your correction factor. You still need to know your insulin timing. You still need to know when to override the suggestion.
How to Start Using Trend Arrows
Step 1: Know your correction factor. Ask your provider. If you don’t know it, you can’t adjust properly.
Step 2: Learn the arrow meanings. Print the Endocrine Society tables. Keep them on your fridge. Use them for a week.
Step 3: Track your results. For two weeks, write down every time you adjusted based on an arrow. What happened 90 minutes later? Did you stay in range? Did you avoid a low?
Step 4: Talk to your provider. Don’t assume they know you’re using this. Show them your data. Ask if your correction factor is still right.
Step 5: Be patient. It takes 3 to 4 weeks to build confidence. Most people give up after a few days because they’re afraid of messing up. But the data says: if you stick with it, you’ll spend more time in range and have fewer scary lows.
CGMs are powerful. But they’re not magic. They’re tools. And like any tool, they work best when you know how to use them. Trend arrows are the most underused feature in diabetes tech. But they’re also the most effective. Stop guessing. Start adjusting. Your next low doesn’t have to happen.

Cara C
December 21, 2025 AT 05:51I started using trend arrows last month and honestly? My nighttime lows dropped by like 70%. I used to wake up at 3 AM panicking, now I sleep through the night. It’s not magic, it’s just paying attention to the direction, not just the number.
Also, I print the Endocrine Society chart and tape it to my insulin pump. Old school, but it works.
Grace Rehman
December 21, 2025 AT 18:54So you’re telling me the government and Big Pharma don’t want you to know you can avoid hypoglycemia by reading arrows instead of blindly injecting insulin? Of course they don’t. Why sell more pens when you can teach people to think?
They’ll call it ‘patient empowerment’ but really it’s just them losing control. The real cure isn’t in a vial-it’s in the data you’re already holding.
Jerry Peterson
December 23, 2025 AT 08:49Been using CGM arrows for two years now. My kid with T1D went from 4 lows a week to maybe one a month. The pediatric dosing adjustments? Total game changer. You don’t need to be a scientist-just follow the damn arrows and trust the trend.
Also, if your provider hasn’t told you this, ask for a diabetes educator. They’re not optional.
Adrian Thompson
December 24, 2025 AT 17:56CGMs? Trend arrows? This is all just another way to track you. Dexcom, Abbott, Medtronic-they’re feeding your data to the government. You think they care about your blood sugar? They care about your biometrics. This isn’t healthcare. It’s surveillance with a side of insulin.
And don’t get me started on the 2024 ADA guidelines. Who funded that? Who signed the papers? Ask yourself who profits when you’re ‘adjusted’ every 5 minutes.
Southern NH Pagan Pride
December 26, 2025 AT 02:50the arrows r just a distracation... the real issue is the glyphosate in our food making our livers misread glucose... the cgm is just a cover for the real problem: chemtrails and fluoridated water messing with your endocrine system.
why do you think all the big pharma companies sponsor these 'guidelines'? they want you addicted to the tech so you never question the poison in your soda.
Jay lawch
December 26, 2025 AT 05:20Let me tell you something about this so-called science. In India, we have been managing diabetes for centuries with Ayurveda, fasting, and mindful eating. Why are we now bowing down to American corporate algorithms that tell us to add 1.2 units based on some sensor reading? This is cultural imperialism disguised as medicine.
My grandfather never saw a CGM. He lived to 92. He ate bitter gourd, walked 10 kilometers daily, and never once took insulin. But now, because some white-coated tech bros in Silicon Valley say trend arrows are the future, we are abandoning our own wisdom. This is not progress. This is surrender.
Dan Adkins
December 26, 2025 AT 12:29While I acknowledge the empirical validity of the trend arrow methodology as articulated in the Endocrine Society guidelines, I must emphasize the necessity of contextual calibration within the framework of individual metabolic variability. The assumption that a fixed unit adjustment applies universally neglects the dynamic interplay of cortisol rhythms, circadian insulin sensitivity, and glycogen storage kinetics.
Furthermore, the reliance on proprietary sensor algorithms introduces a significant epistemological vulnerability. One must interrogate the calibration protocols and potential algorithmic bias inherent in these commercial platforms. This is not merely a clinical recommendation-it is a systemic dependency.
Erika Putri Aldana
December 27, 2025 AT 04:36Bro this is just a fancy way to say 'guess more'. I tried it for a week and ended up in the ER because I trusted a stupid arrow. Now I just use my meter and eat a snack if I feel shaky. Why make it harder?
Also why do people act like this is new? My grandma did this with her fingers and a notebook in the 80s 😒
Jon Paramore
December 28, 2025 AT 13:25Correction factor 1:50? Double-down arrow? Add -1.2 units. That’s it. No math. No guesswork. Just follow the algorithm.
Pro tip: Always check IOB first. I’ve seen people double down on insulin because they forgot their last bolus was still active. That’s how you get a 38 mg/dL low at 2 AM.
Also-yes, this works for SGLT2 users too. Saw a patient with euglycemic DKA last month. CGM showed flat, ketones up. Dose reduced. No hospital. Simple.
Swapneel Mehta
December 29, 2025 AT 06:23I didn’t believe in arrows until I saw my glucose drop 40 points in 20 minutes after eating because I didn’t adjust. Now I look at the arrow before every meal. It’s like having a co-pilot.
Also, the pediatric adjustments? My niece went from 3 night lows a week to zero. Her mom cried. I cried. It’s not tech magic. It’s just better info.
Cameron Hoover
December 29, 2025 AT 07:19Just saw my CGM go double-down after lunch. I cut my insulin by 1.2 units. Sat there. Waited. Watched it level out. No crash. No panic. No ER.
That one moment? That’s why I don’t ever go back to fingersticks. This isn’t just data. It’s peace of mind.