What Is Drug Allergy Skin Testing?
Drug allergy skin testing is a safe, simple way to find out if you’re truly allergic to a medication. It’s not a guess. It’s not a guess based on what you felt years ago. It’s a direct test that looks at how your skin reacts to tiny amounts of the drug. If you’ve been told you’re allergic to penicillin, amoxicillin, or another medicine-and you’ve avoided it ever since-this test might prove you’re not allergic at all. That’s not just convenient. It could mean better treatment, fewer side effects, and lower healthcare costs.
Doctors don’t use this test for every drug. It works best for certain types of reactions, especially those that happen quickly-within minutes to an hour after taking the medicine. Think rashes, hives, swelling, trouble breathing, or even anaphylaxis. These are called immediate reactions. Skin testing is most accurate for beta-lactam antibiotics like penicillin and amoxicillin. For other drugs, like NSAIDs or sulfa drugs, it’s less reliable.
How Does It Work?
There are three main types of skin tests, and your doctor will pick the right one based on the drug and your history.
- Skin prick test: A drop of the drug solution is placed on your skin-usually your forearm or back. A tiny needle lightly pricks through the drop, letting a small amount of the drug enter just below the surface. It feels like a quick mosquito bite.
- Intradermal test: If the skin prick is negative, your doctor might follow up with this. A small amount of the drug is injected just under the skin with a fine needle. It creates a tiny bump, like a mosquito bite you can feel more clearly. This test is more sensitive but can also give false positives.
- Patch test: Used for delayed reactions that show up hours or days later. A patch with the drug is taped to your skin for 48 hours. You come back to have it checked for redness or swelling.
Every test includes two controls: one with histamine (which should make your skin react) and one with saline (which shouldn’t). If the histamine doesn’t cause a bump, the test is invalid. If the saline causes a reaction, your skin might be overly sensitive, and results can’t be trusted.
What Should You Do Before the Test?
Preparation matters. If you’re taking antihistamines-like cetirizine, loratadine, or diphenhydramine-you need to stop them at least five to seven days before testing. These meds block your body’s allergic response, so they can hide a real allergy. That means your test might come back negative even if you’re allergic.
Don’t stop any other medications unless your doctor tells you to. If you’re on beta-blockers or ACE inhibitors for high blood pressure, let your provider know. These can interfere with how your body handles a reaction, and they might make treatment harder if something goes wrong.
Also, avoid applying lotions, creams, or oils to your arms or back on the day of the test. Oily skin can make it harder for the drops to stay in place.
What Happens During the Test?
The whole process takes about 45 to 60 minutes. You’ll sit in a chair while a nurse or allergist marks your skin with a permanent marker-each spot labeled with the drug being tested. For the skin prick test, they’ll place the drops and lightly prick the skin. You might feel a tiny sting, but it’s not painful.
For intradermal tests, you’ll feel a small pinch and a slight burning or stinging sensation that lasts a few minutes. One patient described it as “like a bee sting that fades fast.”
After each test, you wait 15 to 20 minutes. Your skin is checked for redness, swelling, or raised bumps called wheals. A positive result means the area is bigger than the control and looks like a mosquito bite that’s gotten worse. The size matters. A wheal 3 mm or larger than the saline spot is considered positive.
Doctors take photos of the results. Why? Because skin reactions fade. Having a picture helps future doctors understand your history.

Is It Safe?
Yes-when done correctly. The amount of drug used is tiny. It doesn’t go into your bloodstream. It stays in the top layer of your skin. That’s why serious reactions are extremely rare.
Still, testing is always done in a medical setting with trained staff who can handle anaphylaxis. They have epinephrine, oxygen, and emergency equipment ready. You’ll be watched closely during and after the test.
You won’t be tested if you’re having an active allergic reaction, or if you have uncontrolled asthma. That’s not the time to test-you’re already in danger.
What Do the Results Mean?
A positive result means you’re likely allergic to that drug. You should avoid it in the future. But a negative result doesn’t always mean you’re safe.
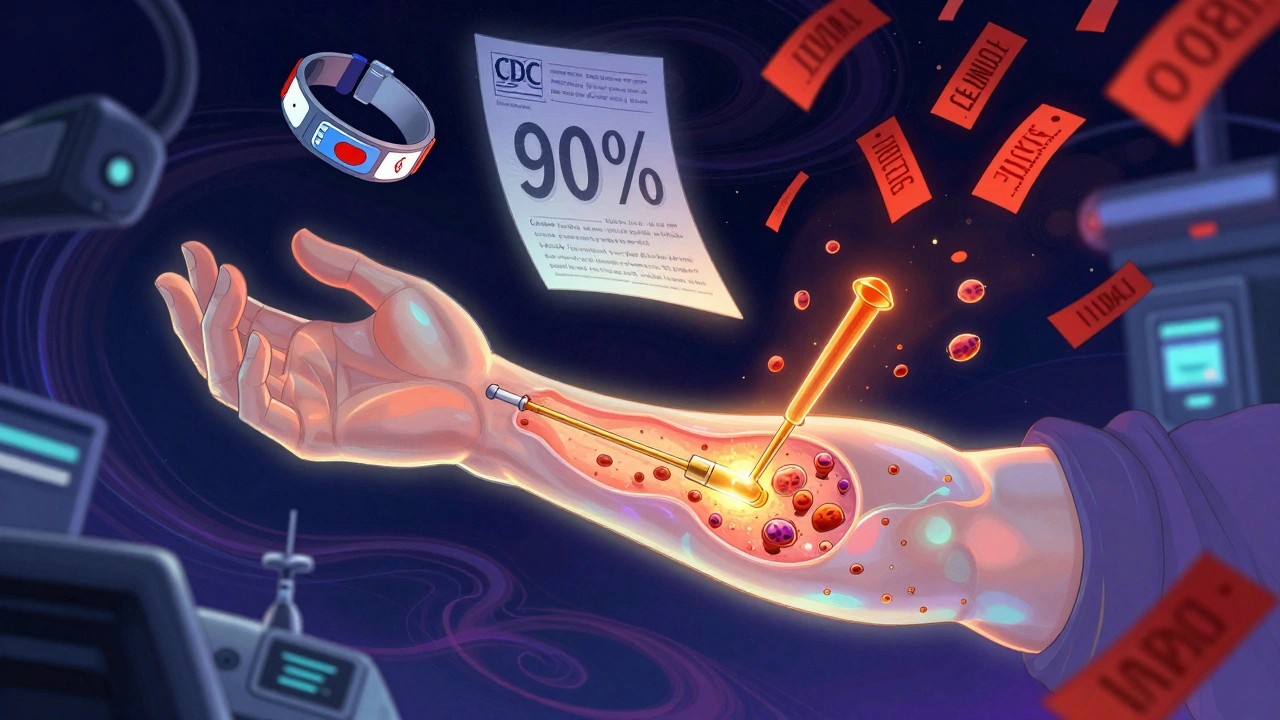
For penicillin, if both the skin prick and intradermal tests are negative, there’s a 95% chance you’re not allergic. That’s why so many people who think they’re allergic to penicillin turn out to be fine. A 2022 CDC report found that 90% of people who say they’re allergic to penicillin aren’t. Skin testing helps clear that up.
For other drugs-like cephalosporins, sulfa drugs, or NSAIDs-negative results are less reliable. That’s because the test reagents aren’t as well standardized. In these cases, your doctor might recommend a drug challenge: giving you a small, increasing dose of the drug under close watch. It’s riskier than skin testing, but sometimes necessary.
Why This Matters for Your Health
Many people are labeled allergic to penicillin based on a childhood rash. But penicillin is one of the safest, cheapest, and most effective antibiotics. If you avoid it unnecessarily, doctors turn to stronger, more expensive, and often more toxic drugs like vancomycin or fluoroquinolones. These drugs increase your risk of side effects, antibiotic resistance, and even deadly infections like C. diff.
Hospitals that run formal allergy testing programs have seen a 30% drop in broad-spectrum antibiotic use. That means fewer resistant infections, shorter hospital stays, and lower costs.
Delabeling-removing an incorrect allergy label from your chart-is one of the biggest wins in modern medicine. It’s not just about avoiding a rash. It’s about getting the right treatment, safely.
What If the Test Is Negative?
If your skin test is negative and your doctor believes it’s reliable for the drug in question, they may suggest a drug challenge. This means you’ll take a small dose of the medicine under supervision. You’ll be watched for at least an hour. If nothing happens, you’re cleared.
One case from the Cleveland Clinic involved a 45-year-old woman who avoided all penicillin-based drugs for 20 years because of a childhood rash. Her skin test was negative. She had a drug challenge and took amoxicillin without issue. She now has more treatment options for future infections-and her doctors can avoid unnecessary antibiotics.
What If the Test Is Positive?
If you have a positive result, you’ll be given a medical alert bracelet or card listing the drug you’re allergic to. You’ll learn to avoid it and all related drugs. For example, if you’re allergic to penicillin, you’ll also avoid amoxicillin, ampicillin, and some cephalosporins.
You’ll also learn what to do if you accidentally take it. Carry an epinephrine auto-injector if your doctor recommends it. Know the signs of anaphylaxis: swelling of the throat, wheezing, dizziness, rapid pulse. Don’t wait. Use your injector and call for help.
Where Can You Get Tested?
Not every clinic offers this. You need an allergist or immunologist trained in drug allergy testing. In the UK, NHS allergy clinics offer it, especially for penicillin. In the US, major hospitals and university medical centers are more likely to have the resources.
Ask your GP or pharmacist to refer you. If you’ve had a severe reaction in the past, you should be referred automatically. Don’t wait until you need antibiotics again. Get tested now.
What’s New in Drug Allergy Testing?
Standardized test kits for penicillin are now approved in Europe and the US. Before, reagents varied between labs, making results inconsistent. Now, hospitals use the same reagents, so results are more reliable.
Researchers are working on better tests for other drugs. Clinical trials are underway for skin test reagents for ciprofloxacin, vancomycin, and even opioids. That’s huge-opioid allergies are often misdiagnosed, and people end up in chronic pain because they’re denied pain meds they could safely take.
Combining skin testing with blood tests (like component-resolved diagnostics) is also improving accuracy. This isn’t routine yet, but it’s coming.
Final Thoughts
If you’ve been told you’re allergic to a drug, ask: Is that based on a test-or a guess? Skin testing gives you real answers. It’s safe. It’s quick. It could change how you’re treated for the rest of your life. You don’t have to live with a label that might be wrong.
Don’t assume you’re allergic. Get tested. Your next infection-and your next antibiotic-could be better because of it.


nina nakamura
December 13, 2025 AT 16:56Constantine Vigderman
December 14, 2025 AT 11:12Cole Newman
December 15, 2025 AT 21:59Tom Zerkoff
December 15, 2025 AT 22:17Alvin Montanez
December 17, 2025 AT 12:12Lara Tobin
December 19, 2025 AT 07:58Jamie Clark
December 20, 2025 AT 23:58Keasha Trawick
December 21, 2025 AT 11:24Sheldon Bird
December 22, 2025 AT 00:05