Drug Combination Risk Checker
Assess Your Risk
This tool estimates the potential danger of combining benzodiazepines with other substances based on FDA guidelines and medical research.
Risk Assessment
Critical Danger
Combining benzodiazepines with opioids or alcohol significantly increases risk of respiratory failure. This combination accounts for 75% of benzodiazepine-related overdose deaths.
High Risk
Mixing with sleep aids or alcohol may cause excessive sedation. Even small amounts of alcohol can be dangerous when combined with benzodiazepines.
Low Risk
No dangerous combinations detected. However, always consult your doctor about long-term use and dependencies.
Note: This tool is for informational purposes only and does not replace medical advice.
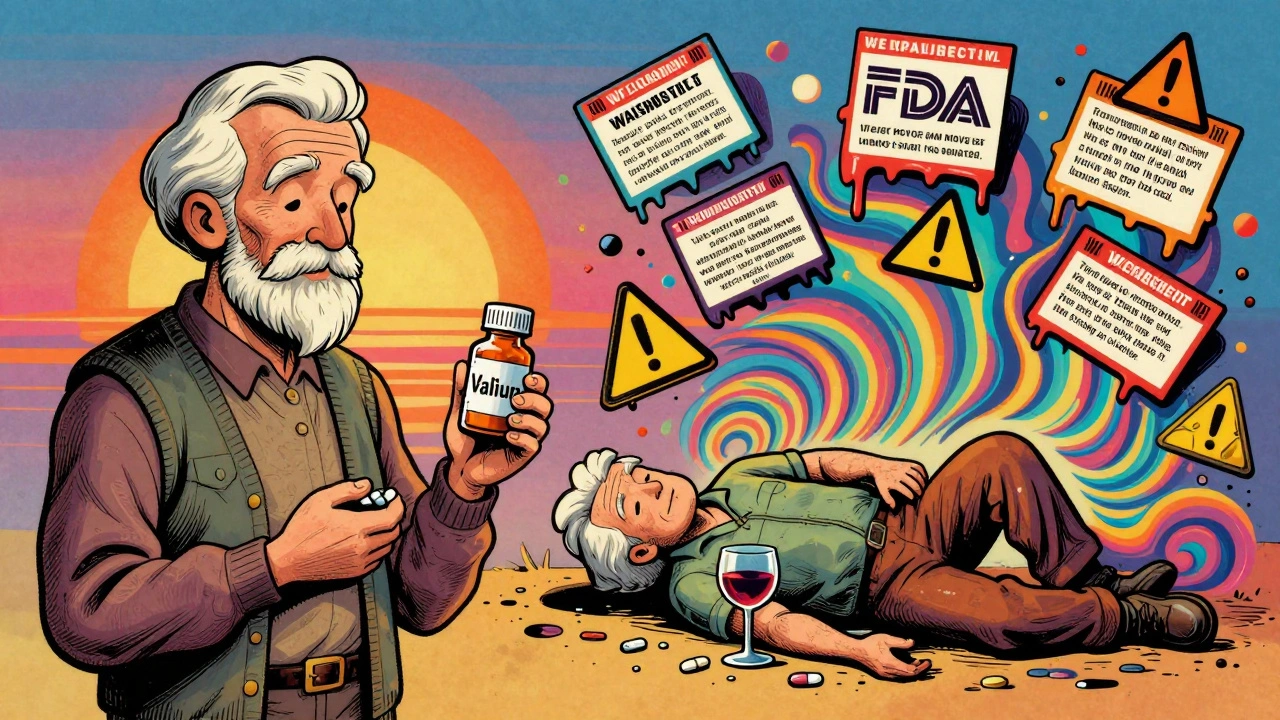
Most people know benzodiazepines like Xanax, Valium, or Ativan as quick fixes for anxiety. They work fast-sometimes in under an hour. But what most don’t realize is how dangerous they can be when taken with other common medications. The FDA issued a boxed warning in 2020 for every benzodiazepine on the market, and it’s not a small print footnote. It’s a red flag: combining these drugs with opioids, alcohol, or even sleep aids can stop your breathing. And it’s not rare.
How Benzodiazepines Actually Work
Benzodiazepines boost the effect of GABA, a calming chemical in your brain. That’s why they reduce panic, help you sleep, and relax tense muscles. But this same mechanism is what makes them risky. When GABA gets overstimulated, your central nervous system slows down too much. Slurred speech, dizziness, confusion-these are early signs. In high doses or with other depressants, it can turn into unconsciousness or respiratory failure.
Not all benzodiazepines are the same. Short-acting ones like alprazolam (Xanax) kick in fast but wear off quickly, making people more likely to take more too soon. Long-acting ones like diazepam (Valium) build up in your system over days. That’s why someone on Valium might feel fine in the morning but crash after a nightcap. The half-life matters. Alprazolam lasts 6-12 hours. Diazepam? Up to 100 hours. That’s why mixing either with another depressant is a gamble-but mixing the short-acting ones is like playing Russian roulette with your breathing.
The Deadliest Combination: Benzodiazepines + Opioids
If you’re taking painkillers like oxycodone, hydrocodone, or fentanyl, and your doctor also gave you Xanax for anxiety, you’re in a high-risk group. The FDA found that 75% of benzodiazepine-related overdose deaths between 2011 and 2016 involved opioids. That’s not coincidence. It’s chemistry. Both drugs depress the brainstem-the part that controls breathing. Together, they don’t just add up. They multiply. Studies show a 15-fold increase in fatal overdose risk compared to opioids alone.
Real cases back this up. One Reddit user, u/AnxietyWarrior2020, described being prescribed Xanax for panic attacks while already on oxycodone for back pain. Within two weeks, he stopped breathing during sleep and ended up in the ICU. A 2017 JAMA study found patients on both drugs had a 154% higher risk of overdose than those on opioids only. These aren’t outliers. They’re predictable outcomes.
Alcohol Makes It Worse-Even in Small Amounts
You’ve heard it before: don’t drink on Xanax. But how many people still do? A 2022 survey by the Anxiety and Depression Association of America found that nearly 1 in 5 benzodiazepine users admitted to drinking alcohol while on the medication. And it’s not just about getting drunk. Even one glass of wine can push someone into dangerous sedation. Alcohol and benzodiazepines hit the same brain receptors. They don’t just add up-they amplify each other. That’s why ER doctors see so many patients passed out after a dinner with wine and a prescribed Ativan.
One Drugs.com review from a pharmacy student described seeing multiple near-fatal cases where people mixed alcohol with benzos. “They didn’t think it was a big deal,” the reviewer wrote. “They thought, ‘I’ve had a drink before, and I’m on this med-I’m fine.’ Then they wake up in the hospital.”
What About Sleep Meds and Antidepressants?
Many people take benzodiazepines for sleep, especially if they’re also on antidepressants. But here’s the catch: SSRIs like sertraline or escitalopram don’t interact dangerously with benzos. They’re often prescribed together. The real danger comes from sleep aids like zolpidem (Ambien) or eszopiclone (Lunesta). These are called Z-drugs, and while they’re not technically benzodiazepines, they work the same way. Mixing them with Xanax or Klonopin is like doubling down on CNS depression.
Older adults are especially vulnerable. The American Geriatrics Society warns against benzodiazepines in people over 65 because they increase fall risk by 50%. When combined with other sedating meds-like muscle relaxants, antihistamines, or even some blood pressure pills-that risk triples. One 2019 study in the Journal of the American Geriatrics Society found that seniors on multiple sedating drugs were far more likely to break a hip or suffer a head injury from a fall. And those injuries often lead to long-term disability or death.
Why Are Doctors Still Prescribing Them?
It’s not that doctors are careless. Many are stuck between a patient in acute panic and limited options. Benzodiazepines work fast. SSRIs take 4-6 weeks. For someone having daily panic attacks, waiting isn’t an option. But the problem is long-term use. About 40% of people who take benzodiazepines for more than six months develop physical dependence. Quitting cold turkey can trigger seizures, hallucinations, or extreme anxiety. Tapering off requires weeks or months, and many patients aren’t given a plan.
And here’s the kicker: only 43% of primary care doctors routinely check for benzodiazepine-opioid combinations, even after the FDA’s 2020 warning. Many patients don’t even know they’re on two dangerous drugs. They see different specialists-one for pain, one for anxiety-and no one connects the dots.

What Should You Do If You’re on Benzodiazepines?
First, don’t panic. If you’re taking them as directed and not mixing them with other depressants, you’re likely okay. But you need to be proactive.
- Review all your meds with your doctor or pharmacist. Include over-the-counter sleep aids, cold medicines, and supplements. Even melatonin can add up if you’re already sedated.
- Never drink alcohol while on benzodiazepines. Not even a glass of wine. Not even if you feel fine.
- Ask if you really need it. Is this for a panic attack after surgery? Maybe. Is this for daily stress for the last three years? That’s a red flag.
- Get a taper plan if you’ve been on it longer than a few weeks. Don’t stop on your own. Withdrawal can be life-threatening.
The American Psychiatric Association now says benzodiazepines should be a last resort after SSRIs or therapy. They recommend limiting use to four weeks max. That’s not because they’re useless-it’s because safer, longer-term options exist.
The Bigger Picture: A Shift in Treatment
Prescriptions for benzodiazepines have dropped from 13.1% of U.S. adults in 2013 to 10.8% in 2021. Why? Because people are waking up. More patients are asking for therapy, mindfulness, or SSRIs. More doctors are listening. States with prescription monitoring systems that flag benzo-opioid combos have seen a 27% drop in dangerous pairings within 18 months.
Meanwhile, SSRIs are now prescribed for 68% of new anxiety cases, compared to just 22% for benzodiazepines. That’s a major shift. The future isn’t about stronger sedatives. It’s about smarter, safer, longer-lasting solutions.
Benzodiazepines still have a place. They can save lives in acute crises-like severe panic during a medical emergency or alcohol withdrawal. But they’re not meant to be daily crutches. And they’re absolutely not meant to be mixed with anything that slows your breathing.
What If You’ve Already Mixed Them?
If you’ve taken benzodiazepines with opioids, alcohol, or sleep meds and feel unusually drowsy, confused, or have trouble breathing, call 911. Don’t wait. Don’t try to sleep it off. This isn’t a bad hangover. It’s a medical emergency.
If you’re worried you might be dependent or have been taking them too long, talk to your doctor about a taper plan. Don’t quit cold turkey. And if your doctor doesn’t take your concerns seriously, find someone who does. Your life depends on it.


Paul Dixon
December 12, 2025 AT 07:10Man, I had no idea mixing Xanax with a beer could be this deadly. I thought it was just a myth people made up to scare others. My cousin did it for years and never had an issue… until she didn’t. She woke up in the hospital after a dinner with wine and her nightly Klonopin. Scared the hell out of me. Never touch alcohol with these meds. Period.
Katherine Liu-Bevan
December 13, 2025 AT 08:20As a pharmacist, I see this every single day. Patients come in with 5 different prescriptions, none of which their doctor reviewed together. Benzodiazepines + opioids + sleep aids + muscle relaxants = a walking overdose. The FDA warning is loud, but doctors are overworked and patients don’t know to ask. Always bring a full med list to every appointment-even the OTC stuff like NyQuil or melatonin. It adds up faster than you think.
Eddie Bennett
December 14, 2025 AT 17:40I’ve been on Xanax for 4 years. Not because I wanted to, but because my therapist said I wasn’t ready for SSRIs yet. Tapering off is hell. I cried for three weeks straight. But I’m down to 0.25mg a day now, and I finally sleep without it. Don’t let anyone tell you it’s ‘just anxiety.’ This stuff rewires your brain. You need a plan. Don’t wing it.
Aman deep
December 16, 2025 AT 10:09Bro, I’m from India and we don’t even have benzos as easy as here. We got ayurveda, yoga, chai, and a whole lot of ‘just breathe.’ But I’ve seen friends in the US go down this road. It’s not weakness-it’s a system failure. Doctors hand out scripts like candy and never follow up. We need better mental health infrastructure, not just more pills.
Jean Claude de La Ronde
December 16, 2025 AT 17:29So let me get this straight… we’ve got a drug that turns your brain into a slow-mo movie, and instead of fixing the root cause of anxiety, we just turn up the sedative dial? Genius. Next they’ll prescribe sleeping pills for climate anxiety. At least we’re honest about it-‘Here, take this and forget the world exists.’ Real solution: get a dog, go for a walk, talk to someone who doesn’t charge $200/hour.
Vivian Amadi
December 16, 2025 AT 21:41Anyone who takes benzos long-term is just weak. You don’t need meds-you need discipline. I’ve never taken one and I’ve survived divorce, job loss, and my cat dying. You’re choosing to be helpless. Stop blaming doctors. Stop blaming the system. Just grow up.
Courtney Blake
December 17, 2025 AT 03:17Oh great, another ‘dangerous drug’ article. Let me guess-next you’ll tell me coffee causes anxiety? I’ve been on Valium for 15 years, drink two glasses of wine every night, and I’m fine. My liver’s stronger than your fear-mongering. This is just more fear porn to sell therapy subscriptions. Wake up.
Lisa Stringfellow
December 18, 2025 AT 21:29Wow, so now we’re blaming patients for being prescribed dangerous combos? What about the doctors who don’t check interactions? What about the pharma reps pushing these drugs? You act like it’s the patient’s fault they didn’t read the 87-page insert. Newsflash: most people don’t. And if they did, they’d still take it because they’re desperate. Stop victim-blaming and fix the system.
Monica Evan
December 19, 2025 AT 22:02I’m a nurse and I’ve seen the aftermath. A 72-year-old woman on Xanax, Ambien, and hydrocodone for arthritis fell in the shower, cracked her skull, and never woke up. She wasn’t ‘abusing’ anything. She was just following orders. Her doctor didn’t know she was on three CNS depressants. We need better communication between specialists. And we need to stop treating anxiety like a broken lightbulb you just swap out.
Jim Irish
December 21, 2025 AT 04:36Respectfully, this is a critical public health issue. The data is clear. The risks are quantifiable. The solutions are known. What’s lacking is coordination. Patients are falling through the cracks because care is fragmented. We need electronic health record alerts, mandatory interaction checks, and standardized patient education. This isn’t about fear. It’s about responsibility.
Sylvia Frenzel
December 22, 2025 AT 07:23Why do we even have these drugs if they’re so dangerous? Just ban them. We don’t need them. Therapy is better. Exercise is better. Why are we still letting Big Pharma push this? It’s not medicine-it’s chemical pacification. And it’s destroying families.
Taylor Dressler
December 23, 2025 AT 12:30I’ve been off benzos for two years now. Started with therapy, then SSRIs, then mindfulness. It took time. I had bad days. But I didn’t lose my job, my relationships, or my breathing. I’m not saying it’s easy. But it’s possible. And it’s worth it. You don’t have to live in a fog.
Aidan Stacey
December 24, 2025 AT 15:21My dad took Xanax for 10 years after his heart attack. He didn’t even know he was mixing it with his blood pressure meds. One night he stopped breathing. We didn’t know why until the ER doc pulled up his med list. He’s fine now, but he’s on therapy and walks every morning. No pills. No booze. Just him, his dog, and the sunrise. It’s not glamorous. But it’s real.
Mia Kingsley
December 26, 2025 AT 05:18LOL this whole post is just fearmongering. I’ve taken Xanax with wine for 8 years and I’m still alive. You think I’m gonna stop because some article says ‘don’t’? Nah. I’m not a lab rat. You want to save people? Stop telling them what to do and start listening to them. Some of us need this. Deal with it.