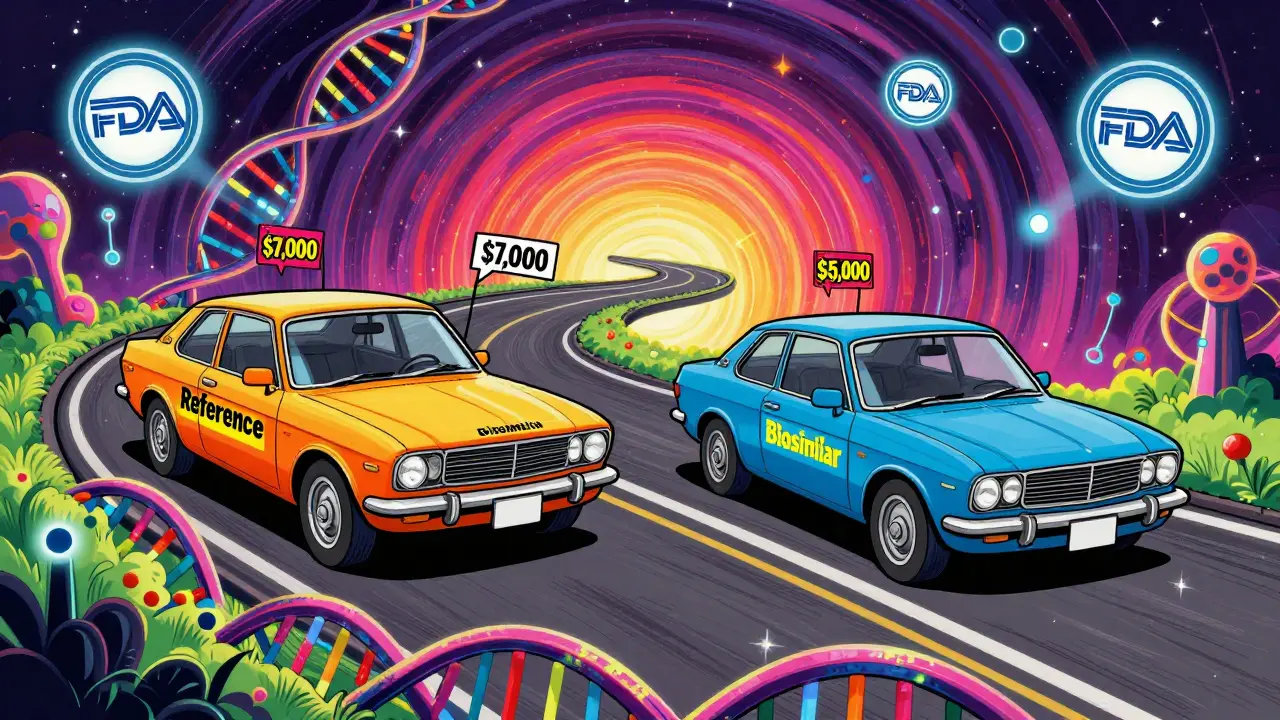
Biologic drugs have changed how we treat serious conditions like rheumatoid arthritis, Crohn’s disease, and certain cancers. But they come with a steep price tag-sometimes over $7,000 a month. That’s why biosimilars have become such a big deal. They’re not generics, but they’re designed to do the same job at a lower cost. If you’ve been told you can switch to a biosimilar, or you’re just trying to make sense of the hype, here’s what you actually need to know.
What Exactly Is a Biosimilar?
A biosimilar is a biologic drug that’s highly similar to an already-approved biologic, called the reference product. It’s not an exact copy. Unlike generic pills, which are made from simple chemicals, biologics come from living cells-yeast, bacteria, or animal cells. That means even tiny changes in the manufacturing process can affect the final product. The FDA requires biosimilars to show no clinically meaningful differences in safety, purity, or potency compared to the original. That’s not marketing speak-it’s science.
Think of it like two identical-looking cars built in different factories. They both run on gasoline, have the same engine specs, and get the same mileage. But one was made in Germany, the other in Japan. The parts might be sourced differently, but the performance? The same. That’s biosimilars in a nutshell.
How Are Biosimilars Approved?
The FDA doesn’t require biosimilars to repeat every single clinical trial done for the original drug. Instead, they use what’s called the “totality of evidence.” That means:
- Extensive lab tests comparing the molecular structure
- Animal studies to check for toxicity
- Human studies showing how the body absorbs and processes the drug
- Comparisons of immune responses and side effects
Only if all these pieces line up does the FDA approve it. The process is stricter than for generics, and that’s by design. You can’t just reverse-engineer a living cell product the way you can with a chemical pill.
As of October 2023, the FDA has approved 45 biosimilars. Most target major biologics used for cancer, autoimmune diseases, and diabetes. The first one, Zarxio (a biosimilar to Neupogen), hit the market in 2015. Since then, the pipeline has filled up fast.
How Much Do Biosimilars Actually Save?
This is where things get messy. You’ll hear “biosimilars cut costs by 30%,” but that’s not the whole story. The list price-the sticker price-might be 15% to 35% lower. But what you pay at the pharmacy? That depends on insurance, rebates, and how pharmacies and insurers negotiate.
Take Humira. Its list price was around $7,000 a month before biosimilars arrived. When the first biosimilars launched in 2023, their list prices were about $5,000. That’s a 28% drop. Sounds great, right? But if your insurance has a high deductible or you’re on Medicare Part D, your out-of-pocket cost might not change much unless the plan actively favors biosimilars.
Here’s the real win: when multiple biosimilars enter the market, prices drop further. In Europe, where competition is less restricted, biosimilars have cut costs by up to 70% over time. In the U.S., that’s still happening-but slower. The Inflation Reduction Act of 2022 helped by capping Medicare Part D cost-sharing for biosimilars at 25% starting in 2024. That means more patients will actually feel the savings.
Studies estimate biosimilars could save the U.S. healthcare system up to $150 billion by 2030. But that only happens if patients and doctors use them. Right now, adoption varies. For infliximab (Remicade), biosimilars took 72% of new prescriptions within 18 months. For etanercept (Enbrel), it was only 28%. Why? Because drugmakers used legal tactics to delay competition.
Are Biosimilars Safe?
Yes. And the data backs it up.
The NOR-SWITCH trial, published in The Lancet in 2016, followed over 500 patients who switched from a reference biologic to a biosimilar. After 52 weeks, there was no increase in side effects, loss of effectiveness, or immune reactions. Other large studies across Europe and the U.S. have confirmed the same.
The FDA states clearly: “Biosimilars are as safe and effective as their reference products.” The European Medicines Agency has tracked biosimilars for over 16 years with no new safety signals.
Still, some patients worry. A 2022 survey by the Arthritis Foundation found 28% of patients were initially concerned about effectiveness. But after talking to their doctors, most of those concerns faded. The biggest issue wasn’t safety-it was confusion.
Can You Just Switch at the Pharmacy?
No. Not like with generics.
When you fill a prescription for a generic version of, say, lisinopril, the pharmacist can swap it out without telling your doctor. That’s because generics are chemically identical.
Biosimilars are different. In 48 U.S. states, a pharmacist can’t substitute a biosimilar for the original biologic unless the prescriber allows it. Even then, some states require the doctor to specify “dispense as written” or “biosimilar substitution permitted.”
There’s also a special category: interchangeable biosimilars. These are approved to be swapped without the prescriber’s involvement. As of November 2023, only six biosimilars had that designation-including Hyrimoz, the first interchangeable version of Humira.
Why the caution? Because biologics can trigger immune reactions. While studies show switching doesn’t increase risk, doctors want to control the process-especially for patients who are stable on their current treatment.
What’s the Patient Experience Like?
Real-world feedback is mostly positive.
On Drugs.com, patients using Renflexis (a biosimilar to Remicade) gave it 4.2 out of 5 stars. Common comments: “Same as Remicade but half the cost,” and “No side effects I didn’t already have.”
Reddit threads in r/rheumatology show patients are still nervous-but also informed. One top-rated comment from a rheumatologist with 2,500+ karma says: “I spend 10 to 15 minutes with every patient explaining the science. Once they understand, most are fine with switching.”
Patients who switched reported 87% saw no difference in effectiveness. And 72% said their out-of-pocket costs dropped. The biggest complaints? Insurance denials and confusing paperwork-not the drug itself.
Why Isn’t Everyone Using Biosimilars?
It’s not about the science. It’s about money and power.
Big drugmakers spend billions protecting their biologic patents. They file lawsuits, tweak formulations slightly to extend exclusivity (“product hopping”), and offer deep rebates to insurers to lock out biosimilars. These tactics delay competition, keeping prices high.
Insurance plans often favor the original biologic because they get rebates from the manufacturer. That means even if a biosimilar is cheaper, the plan might not pass the savings to you.
Doctors, too, face a learning curve. A 2022 ASCO survey found 78% of oncologists needed 1-2 hours of training to feel confident prescribing biosimilars. The biggest hurdle? Navigating payer rules.
And then there’s the lack of clear information. Manufacturer websites often highlight cost savings without explaining how the approval process works. Patients are left guessing.

What’s Next for Biosimilars?
The pipeline is full. Seven biosimilars for Stelara (ustekinumab) are under FDA review. More are coming for key drugs like Enbrel, Orencia, and Humira. By 2027, experts predict biosimilar use will jump from 25-30% to 50-60% for most biologics.
Meanwhile, “biobetters”-next-gen biologics with improved properties-are starting to emerge. These aren’t biosimilars. They’re upgrades. They’ll compete with both the original and biosimilars, adding more choices.
The real game-changer? If the U.S. adopts policies that encourage competition-like limiting patent abuses and requiring transparency in rebates-the savings could be massive. Right now, Europe leads. The U.S. is catching up. But it’s still early.
What Should You Do?
If you’re on a biologic:
- Ask your doctor if a biosimilar is an option for you.
- Call your insurance and ask: “Do you cover biosimilars? What’s my cost if I switch?”
- Don’t assume your out-of-pocket will drop just because the list price did.
- Use trusted sources: FDA’s Purple Book, the Biosimilars Council, or your pharmacist.
- If you’re nervous, ask for data. Show your doctor this article. Ask: “What’s the evidence?”
If you’re not on a biologic yet, and your doctor suggests one: ask if a biosimilar is available. It’s not a compromise. It’s a smart, science-backed choice.
Biosimilars aren’t magic. But they’re not a gamble either. They’re the result of over a decade of research, regulatory rigor, and real-world testing. And for millions of people, they’re making life-changing treatments affordable.
Are biosimilars the same as generic drugs?
No. Generics are chemically identical copies of small-molecule drugs, like aspirin or metformin. Biosimilars are highly similar-but not identical-to complex biologic drugs made from living cells. The manufacturing process for biologics is too complex to copy exactly, so biosimilars undergo much stricter testing than generics.
Can I switch from a biologic to a biosimilar safely?
Yes. Multiple large studies, including the NOR-SWITCH trial with over 500 patients, show no increase in side effects, loss of effectiveness, or immune reactions when switching from a reference biologic to a biosimilar. The FDA and EMA both confirm biosimilars are as safe and effective as the originals.
Why are biosimilars cheaper if they’re just as good?
They’re cheaper because manufacturers don’t have to repeat the full clinical trials done for the original drug. They use existing data to prove similarity, which cuts development costs. Also, competition drives prices down. When multiple biosimilars enter the market, prices drop further-like what happened in Europe with filgrastim.
Will my insurance cover a biosimilar?
It depends. Many insurers now prefer biosimilars because they’re cheaper. But some still favor the original biologic due to rebates. Always check your plan’s formulary. Ask: “Is there a biosimilar for my drug? What’s my copay if I switch?” Don’t assume coverage-it’s not automatic.
What’s the difference between a biosimilar and an interchangeable biosimilar?
An interchangeable biosimilar is a special FDA designation. It means the product can be substituted for the reference drug at the pharmacy without the prescriber’s permission-just like a generic. Only six biosimilars have this status as of late 2023, including Hyrimoz for Humira. All interchangeable biosimilars are biosimilars, but not all biosimilars are interchangeable.
Do biosimilars have fewer side effects?
No. They have the same expected side effects as the reference biologic. Studies show no increase in immune reactions or adverse events. Any difference in side effects is usually due to individual patient factors, not the biosimilar itself.
How long have biosimilars been used?
The first biosimilar, Omnitrope, was approved in the European Union in 2006. The U.S. approved its first biosimilar, Zarxio, in 2015. Since then, over 45 have been approved in the U.S., with more than 16 years of real-world safety data in Europe.
Final Thought
Biosimilars aren’t a compromise. They’re the result of smart science, rigorous regulation, and growing market pressure. The goal was never to replace biologics-it was to make them accessible. And for the first time, millions of patients are getting the same life-saving treatments at a fraction of the cost. The system isn’t perfect. But the evidence is clear: biosimilars work. And they’re here to stay.

Sajith Shams
December 18, 2025 AT 22:13Biosimilars are just a scam dressed up as science. The FDA approval process is a joke-half the time they skip proper immunogenicity studies. I’ve seen patients crash after switching. If it ain’t identical, it ain’t safe. Don’t let Big Pharma fool you with fancy graphs and ‘clinical meaningfulness’-that’s just legalese for ‘we didn’t prove it’s dangerous.’
Meenakshi Jaiswal
December 20, 2025 AT 10:50As a pharmacist in Mumbai, I’ve dispensed biosimilars for 5+ years. Patients save 60-70% on monthly costs-huge when you’re paying out of pocket. No increase in adverse events. The science is solid. The problem? Doctors here still think ‘biosimilar = inferior.’ Education is the real barrier, not safety.
Ashley Bliss
December 21, 2025 AT 04:25Let’s be real-this whole biosimilar movement is just corporate greed wrapped in a lab coat. You think they care about patients? No. They care about profit margins. They’re pushing these drugs because they can’t keep charging $7k/month forever. And now they want you to feel guilty for wanting the ‘original’-like you’re some selfish monster for not switching. Wake up. This isn’t healthcare. It’s capitalism with a stethoscope.
Danielle Stewart
December 21, 2025 AT 19:29I switched from Humira to Hyrimoz last year. My rheumatologist spent 20 minutes explaining the data. I read the NOR-SWITCH paper. I asked about immune reactions. I was nervous-but zero difference in symptoms, energy, or side effects. My copay dropped from $120 to $30. If you’re scared, ask for the evidence. Don’t let fear drive your health decisions.
Connie Zehner
December 22, 2025 AT 09:34Why do you think they’re pushing biosimilars so hard? Because they know the original drugs are barely better than placebos after 5 years. The real story? The biologics are losing efficacy, and they’re using biosimilars to distract you from the fact that the whole system is broken. You’re being used as a guinea pig for corporate cost-cutting. I’ve seen people get worse after switching. No one talks about that.
Matt Davies
December 23, 2025 AT 22:20Imagine if your iPhone 14 was replaced with an ‘iPhone 14 Pro Max Biosimilar’-same screen, same processor, same battery life, but made by a different factory. Would you panic? Nah. You’d be thrilled you saved $300. Biosimilars are the same deal. The science is rock-solid. The fear? Pure marketing noise from companies who got rich off your pain.
benchidelle rivera
December 25, 2025 AT 02:37Let’s not sugarcoat this: insurance companies are the real villains. They get kickbacks from the originator drug makers. Even when biosimilars are cheaper, they steer patients toward the pricier option because the rebate is higher. The system is rigged. Patients aren’t being protected-they’re being exploited under the guise of ‘cost containment.’
Moses Odumbe
December 26, 2025 AT 09:12Just got my first biosimilar prescription (Adalimumab biosimilar). Copay: $15. Original? $110. I did a deep dive-FDA, Lancet, EMA data. Zero red flags. My doc said, ‘If it wasn’t safe, I wouldn’t prescribe it.’ And he’s been doing this for 25 years. 🤝✅ Science wins. Money loses. Let’s go.
holly Sinclair
December 26, 2025 AT 20:33It’s fascinating how we’ve constructed this entire moral panic around biosimilars when the data is overwhelmingly in their favor. Why do we treat biological molecules with such existential dread? We accept variations in food, in wine, in artisanal bread-why not in medicine? The fear isn’t rooted in biology-it’s rooted in our cultural aversion to complexity and our addiction to the myth of perfect, unchanging solutions. Biosimilars force us to confront the truth: medicine is messy, probabilistic, and deeply human. And that terrifies us more than any immune reaction ever could.
Kelly Mulder
December 27, 2025 AT 13:04Let’s be clear: if you’re taking a biosimilar, you’re not getting the same drug. The FDA’s ‘no clinically meaningful difference’ is a legal loophole, not a biological guarantee. And don’t get me started on the ‘interchangeable’ label-that’s just a marketing ploy to make people feel better about taking a second-tier product. Real medicine shouldn’t be a lottery.
Dev Sawner
December 28, 2025 AT 10:41The data from India’s biosimilar market is unambiguous. Over 1.2 million patients treated with biosimilars for TNF inhibitors since 2018. Adverse event rates: 1.2% vs 1.1% for originators. No statistically significant difference. The WHO’s Global Observatory on Biosimilars confirms this. The resistance is ideological, not scientific. Stop letting fear override evidence.
Glen Arreglo
December 29, 2025 AT 22:04I’m an immigrant from Nigeria who’s been on Enbrel for 8 years. My wife’s cousin in Lagos got the biosimilar version for 1/10th the cost. Same results. No hospitalizations. No flare-ups. The only thing different? She sleeps better because she’s not stressed about bills. This isn’t about science-it’s about dignity. Why should an American pay 10x more for the same life-saving treatment? The system is broken. Biosimilars aren’t the problem-they’re the fix.
bhushan telavane
December 31, 2025 AT 09:15Here in India, biosimilars are the only reason my uncle could afford treatment for Crohn’s. He was on the verge of giving up. Now he’s back to coaching his son’s cricket team. No drama. No drama. Just a cheaper drug that works. If you’re worried, talk to your doctor. But don’t let fear silence someone who needs help.
shivam seo
January 2, 2026 AT 09:00USA spends $400B on biologics. Biosimilars? A distraction. Real solution? Nationalize drug pricing. Stop letting corporations play monopoly with human lives. Biosimilars are just a Band-Aid. The real cancer is the patent system. Fix that, or stop pretending you care.
Mahammad Muradov
January 2, 2026 AT 11:52It’s ironic. We demand perfect replication in software, yet we accept ‘highly similar’ in life-saving medicine. The regulatory framework is inconsistent. If a biosimilar is not identical, then it is not equivalent. And if it is not equivalent, then it is not safe. The burden of proof lies with the manufacturers. They have not met it. Not truly.