Every year, thousands of patients in the U.S. get the wrong medication-not because the pharmacist made a mistake, but because the wrong patient was identified. It sounds impossible, but it happens more often than you think. A woman walks into the pharmacy with a prescription for insulin. The system shows her name, date of birth, and a list of allergies. But the name on the label? Not hers. Her real name is Linda Carter. The system pulled up Linda Cartwright. One letter off. One missed check. And now, she’s handed a drug she’s allergic to. This isn’t a movie plot. It’s a real case documented by the Emergency Care Research Institute. And it’s entirely preventable.
Why Two Identifiers? The Simple Rule That Saves Lives
The Joint Commission, the main organization that accredits U.S. hospitals and pharmacies, made this rule back in 2003: always use two patient identifiers before giving any medication. It’s not optional. It’s not a suggestion. It’s a requirement for keeping your license. The two identifiers must be unique to the person-like their full name and date of birth. Or their medical record number and phone number. What doesn’t count? Room number. Floor. Bed number. Even a nickname. These aren’t tied to the person-they’re tied to a location, and locations change. Why does this matter? Because in a busy pharmacy, names get mixed up. Two patients named Michael Smith? Common. One with a birthdate of 03/15/1980? Not rare. Without a second identifier, you’re guessing. And in pharmacy work, guessing kills.What Happens When You Skip the Second Identifier
A 2020 study in JMIR Medical Informatics found that up to 10% of dangerous drug interactions go undetected because patient records are mismatched. That’s about 6,000 people a year getting medications that could cause seizures, organ failure, or death. And it’s not just about allergies. It’s about dosing. A 70-year-old on kidney medication gets a child’s dose because the system confused her with a 7-year-old with the same last name. Or a diabetic gets a beta-blocker-medication that can hide low blood sugar symptoms-because the pharmacist didn’t check the second identifier. The consequences aren’t just medical. They’re legal. In 2023, The Joint Commission found that 28% of all patient safety violations in hospitals were tied to improper patient identification. That’s the third most common reason facilities lost accreditation. And without accreditation? No Medicare or Medicaid payments. For a pharmacy, that means going out of business.Manual Checks Alone Aren’t Enough
You might think: “We just ask the patient their name and birthdate. That’s two identifiers. We’re covered.” But here’s the problem: people lie. People forget. People are confused. Especially when they’re sick, in pain, or on multiple medications. One pharmacist on Reddit shared a story about a patient who gave the wrong birth year because they didn’t remember it. The pharmacist didn’t double-check the medical record. The patient got the wrong blood thinner. They ended up in the ER with internal bleeding. Even worse? Studies show that when pharmacists rely only on verbal confirmation, 42% of the time, the check isn’t even documented. That means if something goes wrong, there’s no proof you did your job. The Joint Commission doesn’t care if you thought you checked. They care if you recorded it.
Technology Makes It Work
The real game-changer? Technology. Barcode scanning at the dispensing counter isn’t fancy-it’s basic. You scan the patient’s wristband. You scan the medication. The system says: “Match.” Or: “No match. Stop.” A 2012 study in the Journal of Patient Safety found that when pharmacies used barcode scanning with patient ID bands, medication errors that reached patients dropped by 75%. That’s not a small number. That’s life or death. Even better? Biometric systems. Some hospitals now use palm-vein scanners. The patient places their hand on a reader. In under 10 seconds, the system pulls up their full record. No asking. No guessing. No typos. A 2024 Altera Health survey found these systems matched patients to records 94% of the time. Without them? Only 17%. And here’s the kicker: EMPI systems-Enterprise Master Patient Indexes-tie all of a patient’s records together across departments. One patient might have five different records because one doctor spelled their name “Maria,” another used “Mary,” and a third used “María.” Without EMPI, you’re working with broken data. With EMPI, you get the full picture: allergies, past reactions, current meds. That’s how you catch a dangerous interaction before it happens.What Community Pharmacies Get Wrong
Hospital pharmacies have the budget for scanners, wristbands, and biometrics. Community pharmacies? Not so much. Most still rely on asking the patient: “What’s your name?” “When were you born?” Then they hand over the pills. No scan. No record. No verification log. A 2023 survey by the American Society of Health-System Pharmacists found that 63% of community pharmacists admitted to cutting corners during busy hours. Why? Because it takes 30 extra seconds to verify. And if you’re filling 150 prescriptions a day, those seconds add up. But here’s what they don’t realize: one mistake can cost you everything. A lawsuit. A license suspension. A reputation destroyed. The solution isn’t more staff. It’s better tools. Even a simple tablet with a barcode scanner costs less than $500. It’s cheaper than one malpractice claim.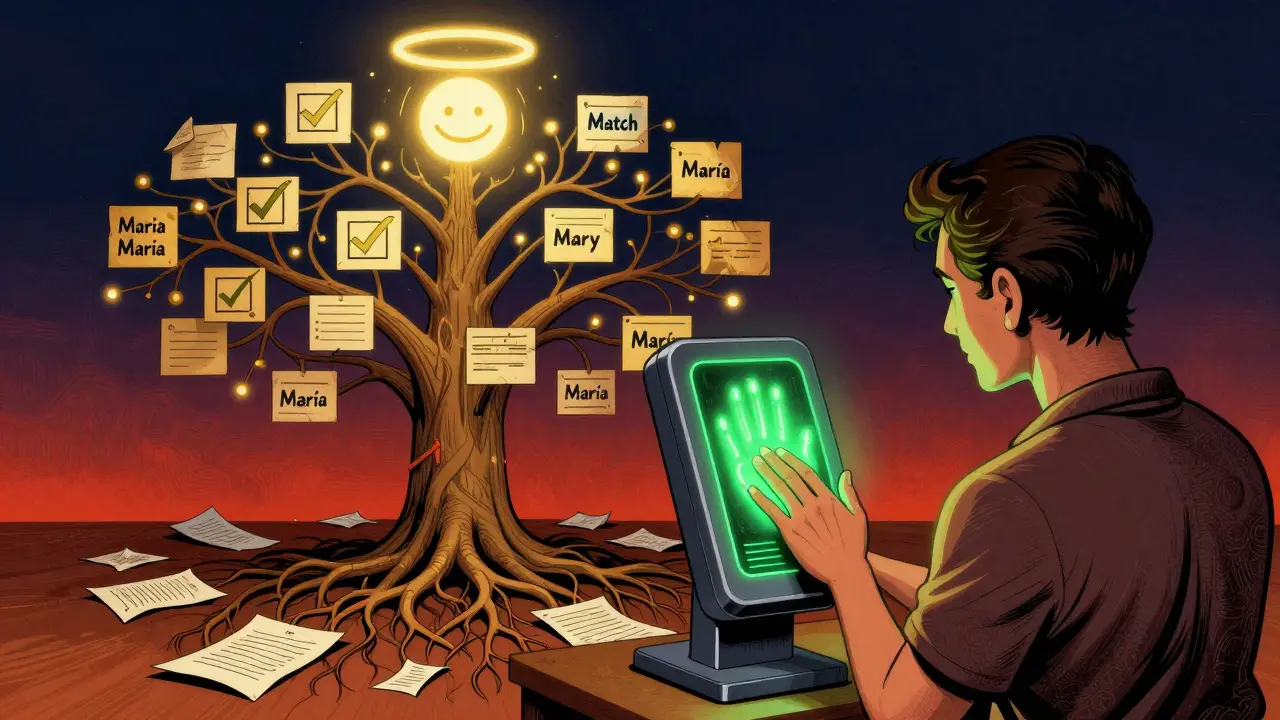
How to Do It Right: A Step-by-Step Guide
If you’re running a pharmacy-or working in one-here’s how to make sure you’re doing this right:- Always use two identifiers-never one. Name + date of birth is the gold standard.
- Never rely on verbal confirmation alone. Even if the patient seems sure, check the system.
- Document the verification. Write it down. Or log it in the system. If it’s not recorded, it didn’t happen.
- Use technology when you can. Even a basic barcode scanner cuts errors by 60% or more.
- Train your staff monthly. Not once a year. Every month. Because habits slip.
- Use timeouts for high-risk meds. Before giving insulin, warfarin, or opioids, pause. Say the two identifiers out loud. Confirm with another pharmacist if possible.
What’s Next? The Future of Patient ID
The Office of the National Coordinator for Health IT is running a pilot in 2025 to test a universal patient identifier-a single number tied to every person in the U.S. healthcare system. Think Social Security number, but for medical records. It’s controversial. Privacy advocates are worried. But the data is clear: without it, we’re still playing Russian roulette with patient safety. In the meantime, the tools we have now are more than enough. Barcode scanners. EMPI systems. Biometric readers. They’re not science fiction. They’re available. Affordable. Proven.Final Thought: It’s Not About Compliance. It’s About Care.
The two-identifier rule isn’t there because bureaucrats wanted more paperwork. It’s there because people died. And they kept dying. Because someone didn’t check the second name. Didn’t scan the wristband. Didn’t log the verification. You’re not just filling prescriptions. You’re holding someone’s life in your hands. And if you’re not using two identifiers every single time-you’re not just breaking a rule. You’re risking a life.What are the two acceptable patient identifiers in a pharmacy?
The Joint Commission requires two unique identifiers tied directly to the patient. Acceptable ones include full name, date of birth, medical record number, or phone number. Room number, bed number, or location are never acceptable because they don’t identify the person-just where they are.
Is asking a patient their name and birthdate enough?
It’s the minimum, but it’s not reliable. Patients can misremember, misunderstand, or give incorrect information. The safest approach is to verify those details against the pharmacy’s electronic record or a scanned ID band. Never rely on verbal confirmation alone.
Why don’t all pharmacies use barcode scanning?
Cost and workflow resistance. Community pharmacies often operate on tight margins and fear slowing down service. But studies show barcode scanning reduces medication errors by 75% and pays for itself by preventing lawsuits and regulatory fines. The real cost is in not using it.
What happens if a pharmacy doesn’t follow the two-identifier rule?
The Joint Commission can deny or revoke accreditation. Without accreditation, the pharmacy loses eligibility for Medicare and Medicaid payments. In severe cases, state boards may suspend or revoke the pharmacist’s license. Legal liability for patient harm is also significantly higher.
Can duplicate patient records cause medication errors?
Yes. One patient can have multiple records if their name is spelled differently across systems. A 2023 ONC report found 8-12% of patient records in U.S. hospitals have duplicates. This means a patient’s allergy history might be hidden in another file. EMPI systems fix this by linking all records under one unique identifier.
Is double-checking by two pharmacists effective?
No. A 2020 review in BMJ Quality & Safety found no strong evidence that having two pharmacists independently check medications reduces errors. The problem isn’t the number of people checking-it’s whether they’re checking the right things. Two people relying on the same flawed system still make the same mistake.
What’s the biggest barrier to implementing two-identifier systems?
Time. Pharmacists feel pressured to move quickly, especially during peak hours. But the real issue is lack of technology. Manual verification takes longer and is less reliable. Investing in barcode scanners or biometric tools reduces time per verification and increases safety.


Emma Addison Thomas
January 8, 2026 AT 02:56Interesting piece. In the UK, we’ve had similar issues with patient misidentification, especially in busy A&E departments. The NHS now mandates two identifiers too, but enforcement varies wildly between trusts. I’ve seen pharmacists just glance at the name and hand over scripts-scary stuff.
What’s wild is how many systems still don’t auto-flag duplicate names. A simple algorithm could prevent half the errors.
Mina Murray
January 8, 2026 AT 22:25Let’s be real-this whole two-identifier thing is just government overreach. You think the system’s perfect? Nah. I’ve seen records mixed up because someone’s middle name was spelled ‘Jen’ instead of ‘Jean’ and the AI flipped out. Now they make you fill out a 12-page form just to get Tylenol.
And don’t get me started on EMPI. That’s just a federal database waiting to be hacked. They’re building a national health ID like it’s 1984 and we’re all in a dystopian thriller.
Sai Ganesh
January 10, 2026 AT 17:40Back home in India, we don’t have barcode scanners or biometrics in most pharmacies. But we have something better: trust. The pharmacist knows your face, your mom’s name, your kid’s birthday. We don’t need tech-we need connection.
Still, I get it. In big cities, names get mixed. Maybe a hybrid? Human + tech. Not either/or.
Alex Danner
January 11, 2026 AT 02:2875% reduction in errors with barcode scanning? That’s not a stat-that’s a miracle.
I worked in a community pharmacy for 8 years. We had one scanner. One. And it broke every other week. We’d beg the distributor for a replacement. They’d say ‘We’re out of stock until Q3.’ Meanwhile, Mrs. Delgado got her husband’s blood pressure med because the system confused ‘Maria’ with ‘María’.
It’s not about cost. It’s about priorities. If your pharmacy can’t afford a $500 scanner, you shouldn’t be filling prescriptions. Period.
Poppy Newman
January 12, 2026 AT 06:36Biometric palm scans? 😍 I saw one at a hospital in London last year. You just wave your hand and boom-your whole med history pops up. No more ‘Is it ‘Linda Carter’ or ‘Cartwright’?’ It’s like magic. And so fast. I wish my local CVS had one. 🙏
Anthony Capunong
January 13, 2026 AT 19:49Oh please. You think this is about patient safety? Nah. It’s about liability. Hospitals and pharmacies don’t care if you live or die-they care if they get sued. That’s why they made the rule. Not because they love you. Because they’re scared of lawyers.
And don’t tell me about ‘two identifiers.’ I’ve seen pharmacists copy-paste the same name and DOB from the last patient. It’s a checkbox. Not a safeguard.
Christine Joy Chicano
January 14, 2026 AT 00:20There’s a quiet horror in how casually we normalize patient misidentification. We treat it like a typo in a text message. ‘Oops, wrong Linda.’ But this isn’t a typo. This is a death sentence wrapped in a barcode.
And yet, we still don’t have a universal ID. Why? Because someone’s making money off the chaos. Data brokers. EMR vendors. Insurance middlemen. The system isn’t broken-it’s designed this way.
Adam Gainski
January 14, 2026 AT 10:58My sister’s a pharmacist in Ohio. She told me they started using tablet scanners last year. Turned out the biggest resistance wasn’t from staff-it was from elderly patients. They felt like criminals being scanned. One woman cried because she thought they were tracking her.
Training matters. Tech helps. But you gotta explain why. Not just mandate it.
Anastasia Novak
January 15, 2026 AT 10:10Let’s be honest: most pharmacists are overworked, underpaid, and emotionally exhausted. You want them to pause and verify? Great. But don’t act like it’s a moral failing when they skip it after 12 hours of screaming kids and angry customers.
Blame the system. Not the people. The system is designed to burn them out. Then when they make a mistake? Oh, now you want compliance? Too late.
Jonathan Larson
January 15, 2026 AT 10:17There is a profound ethical dimension here that transcends protocol. The act of verifying a patient’s identity is not merely procedural-it is sacramental. In that moment, the pharmacist becomes a guardian of human dignity. To reduce this to a checkbox is to commodify the sacred.
When we treat human beings as data points, we lose not just accuracy-we lose our souls. The two identifiers are not bureaucratic hurdles. They are the first act of reverence in the healing process.
Elen Pihlap
January 15, 2026 AT 12:27My grandma died because they gave her the wrong pill. They didn’t even check her name. Just looked at the bottle. She was 82. She didn’t even know her own birthdate anymore. They said it was ‘an accident.’
It wasn’t an accident. It was negligence. And now I can’t sleep.
Paul Mason
January 16, 2026 AT 12:24Man, I’ve seen this happen. My cousin got the wrong chemo drug because the system mixed her up with someone else. Same last name. Different first. No scan. No verification. Just ‘Hey, you’re Karen, right?’
She’s fine now. But her hair never grew back right. And the pharmacy? Still open. No fines. No apology. Just ‘We’re sorry for your trouble.’
LALITA KUDIYA
January 17, 2026 AT 12:41in india we dont have scanners but we have family who come with patients. they know the name, the date, even the doctor. its not tech, its trust. :)
but yes, in cities its a mess. maybe a simple app where patient can show qr code from phone? easy, cheap.
Katrina Morris
January 19, 2026 AT 05:00My cousin works at a pharmacy and they just started using a tablet scanner. It’s so much faster now. No more asking people their birth year-just scan and go. I used to think it was overkill, but now I get it. Safety > speed. 😊