Insomnia Isn’t Just Trouble Sleeping - It’s a Warning Sign
If you’ve been lying awake for hours, tossing and turning while your mind races with worries, you’re not alone. But what if that sleepless night isn’t just stress - it’s a sign your mental health is in trouble? Research now shows that chronic insomnia isn’t just a side effect of depression or anxiety. It’s a major driver of both. People with long-term sleep problems are 40 times more likely to develop severe depression than those who sleep well. That’s not a coincidence. It’s a signal.
Why Treating Sleep Isn’t Optional - It’s Essential
For years, doctors treated depression and anxiety first, hoping sleep would fix itself. But that approach often failed. Patients felt better emotionally, but their sleep stayed broken. And when sleep doesn’t improve, depression comes back. Studies show that treating insomnia alongside depression cuts relapse risk by up to 50%. That’s huge. It means fixing your sleep isn’t a bonus - it’s part of the cure.
The key? Cognitive Behavioral Therapy for Insomnia, or CBT-I. This isn’t a pill. It’s a structured, evidence-backed program that rewires how you think and behave around sleep. Unlike sleeping pills that only mask the problem, CBT-I fixes the root causes. And it works - even when other treatments haven’t.
What Is CBT-I? The Four Core Tools
CBT-I is built on four proven techniques, delivered over 6 to 8 weeks. Here’s how each one works:
- Stimulus Control: Your bed is only for sleep and sex. No scrolling, no working, no watching TV in bed. If you’re not asleep in 20 minutes, get up. Go sit in another room until you feel sleepy. This retrains your brain to associate bed with sleep, not stress.
- Sleep Restriction: You’re probably spending too much time in bed awake. CBT-I cuts your time in bed to match how much you actually sleep. If you’re only sleeping 5 hours, you’re only allowed 5 hours in bed - even if you feel tired. It sounds harsh, but it builds sleep pressure. Soon, you fall asleep faster and stay asleep longer.
- Relaxation Training: Anxiety keeps your body wired. Techniques like diaphragmatic breathing and progressive muscle relaxation calm your nervous system. Just 10 minutes a day can lower cortisol and heart rate, making sleep possible.
- Cognitive Therapy: You might believe, “If I don’t get 8 hours, I’ll collapse tomorrow.” Or, “I’ll never sleep again.” These thoughts keep you alert. CBT-I helps you challenge them with facts. You learn that 6 hours of quality sleep is often enough. And that worrying about sleep is what’s keeping you awake.
Most people start feeling better within 3 weeks. By week 6, 70% of users report significant improvement. And the gains stick - unlike with pills.
CBT-I vs. Sleeping Pills: Why One Works, the Other Doesn’t
Doctors still prescribe zolpidem (Ambien) or similar drugs for insomnia. They work - for a few nights. But here’s the catch: they don’t fix the thinking or habits that caused the problem. Once you stop taking them, insomnia returns. And worse - long-term use can make anxiety and depression worse.
A 2025 study in Nature Scientific Reports compared CBT-I and zolpidem in people with depression and insomnia. Both improved sleep at first. But after six months, only the CBT-I group kept their gains. The pill group was back to square one. CBT-I also reduced anxiety symptoms more deeply. Why? Because it changes your brain’s response to stress - not just your sleep schedule.
And here’s the kicker: CBT-I lowers your risk of developing depression in the first place. One study found that people who completed CBT-I and achieved full insomnia remission were 83% less likely to develop major depression later. That’s prevention - not just treatment.
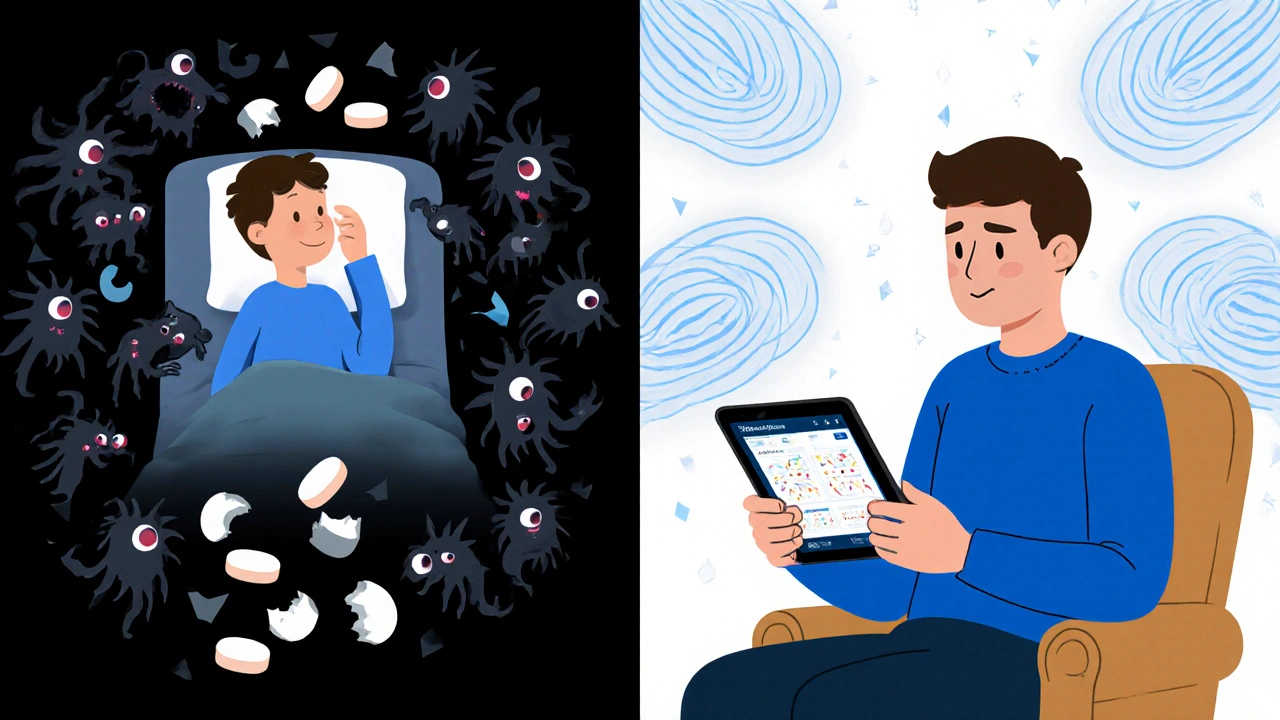
Digital CBT-I: Therapy in Your Pocket
You don’t need to see a specialist in person. Digital platforms like Sleepio and SHUTi deliver full CBT-I programs through apps. These are backed by the same research as in-person therapy. One study showed that users of digital CBT-I had a 57% lower chance of developing moderate-to-severe depression compared to those who just read sleep tips.
Sleepio has over 150,000 users. Of those, 76% saw a clinically meaningful drop in insomnia severity. That’s not marketing - it’s data. And it’s free or low-cost through many NHS and employer health programs in the UK. If you’re in Bristol, check with your GP - they can refer you to a digital CBT-I program at no cost.
Why Isn’t Everyone Getting CBT-I?
If it’s this effective, why don’t more people get it?
First, most doctors still don’t screen for insomnia. They ask, “Are you depressed?” but not, “Are you sleeping?” That’s changing - Kaiser Permanente now screens all depression patients for sleep issues. Since 2022, they’ve seen a 22% drop in depression relapse.
Second, there aren’t enough trained therapists. Only 1-2% of U.S. psychologists are certified in CBT-I. The UK is better, but access is still patchy. Waitlists can be long.
Third, insurance often won’t cover it. In the U.S., 60-70% of people can’t get reimbursement. In the UK, NHS access varies by region. But digital CBT-I is increasingly available through GP referrals.
And finally - the first few weeks are hard. Sleep restriction means you’re tired. Really tired. About 70% of patients quit early because of this. But if you stick with it, the fatigue fades. And the payoff? Better mood, less anxiety, more energy. It’s worth it.

What If CBT-I Doesn’t Work for You?
Not everyone responds. About 30-40% of people don’t achieve full remission. That doesn’t mean it failed. It means you might need a different approach.
Some people benefit from combining CBT-I with antidepressants. A 2024 JAMA Psychiatry study found that taking sertraline with CBT-I led to 40% higher remission rates than medication alone. This combo works best for people with severe depression and long-term insomnia.
Others need more support - group therapy, mindfulness, or even light therapy. If you’ve tried CBT-I and it didn’t stick, talk to your doctor. There’s another path. But don’t give up on treating your sleep. It’s the foundation.
The Bigger Picture: Sleep as Public Health
The pandemic made things worse. In 2021, one in three people had clinical insomnia - double pre-pandemic rates. Mental health services were overwhelmed. But sleep became the quiet crisis nobody talked about.
Now we know: fixing sleep saves lives. Economic studies show every £1 spent on CBT-I returns £2.50-£3.50 in reduced healthcare costs, fewer sick days, and higher productivity. It’s one of the most cost-effective interventions in mental health.
And it’s scalable. Digital programs can reach thousands at once. Governments and employers are starting to invest. If you’re struggling with sleep and mood, you’re not broken. You’re in a treatable condition - and the solution is right there.
Where to Start Today
- Track your sleep for a week. Write down when you get into bed, when you fall asleep, when you wake up, and how you feel in the morning.
- Stop using your bed for anything but sleep and sex. No phones. No TV. No work.
- Go to bed only when you’re sleepy. Get up if you’re not asleep after 20 minutes.
- Try a free digital CBT-I program. Search for “NHS digital CBT-I” or “Sleepio UK” - many are free with a GP referral.
- Talk to your doctor. Say: “I’m having trouble sleeping, and it’s making my anxiety/depression worse. Can we try CBT-I?”
You don’t need to fix everything at once. Just start with one step. Better sleep isn’t a luxury. It’s the first step back to feeling like yourself again.
Can insomnia cause depression, or is it just a symptom?
Insomnia isn’t just a symptom - it’s a major risk factor. Research shows people with chronic insomnia are 40 times more likely to develop major depression. Treating insomnia reduces the chance of depression starting or coming back, even without antidepressants. This is why experts now treat sleep as a primary target, not just a side effect.
Is CBT-I better than sleeping pills for anxiety and depression?
Yes. Sleeping pills like zolpidem help you fall asleep in the short term, but they don’t fix the thoughts or habits causing the problem. Once you stop taking them, insomnia returns. CBT-I teaches your brain to sleep naturally. Studies show it leads to lasting improvement in both sleep and mood, and cuts depression relapse by up to 50%. It’s the only treatment proven to prevent depression from developing.
How long does CBT-I take to work?
Most people start noticing changes in 2 to 3 weeks. Full improvement usually takes 6 to 8 weeks. The hardest part is the first week - sleep restriction makes you tired. But after that, your sleep becomes deeper and more consistent. The key is sticking with it. People who complete the full program are twice as likely to have lasting results.
Can I do CBT-I on my own without a therapist?
Yes. Digital programs like Sleepio and SHUTi are clinically proven to work just as well as in-person therapy. They guide you through each step with videos, daily tasks, and progress tracking. Many are available for free through the NHS or your employer’s health plan. You don’t need a therapist - just commitment and consistency.
What if I’m already on antidepressants? Can I still do CBT-I?
Absolutely. In fact, combining CBT-I with antidepressants like sertraline leads to 40% higher remission rates than medication alone. CBT-I helps you sleep better, which makes antidepressants work more effectively. Many people find they can reduce their medication dose over time once their sleep improves. Always talk to your doctor before making changes.
Is CBT-I covered by the NHS in the UK?
Yes, but access varies. Many NHS trusts offer digital CBT-I programs like Sleepio through GP referrals. Some areas have in-person CBT-I services through IAPT (Improving Access to Psychological Therapies). Ask your GP: “Can I be referred to a CBT-I program for insomnia linked to my anxiety or depression?” Don’t assume it’s not available - ask specifically.
How do I know if my insomnia is serious enough to treat?
If you’ve had trouble falling or staying asleep at least 3 nights a week for 3 months - and it’s affecting your mood, focus, or energy - then yes, it’s serious. You don’t need to wait until you’re in crisis. Early treatment prevents worse problems. Even if your depression feels mild, untreated insomnia will make it worse over time.
Can children or teens benefit from CBT-I for anxiety and depression?
Yes. CBT-I is adapted for teens and children, with simpler language and parental involvement. Sleep problems are a major factor in adolescent depression and anxiety. Studies show CBT-I improves both sleep and mood in teens, often more than medication. If your child is struggling with sleep and mood, ask their GP or school counselor about pediatric CBT-I options.


Iska Ede
November 17, 2025 AT 07:23Gabriella Jayne Bosticco
November 18, 2025 AT 06:26Sarah Frey
November 19, 2025 AT 12:14Katelyn Sykes
November 19, 2025 AT 19:46Gabe Solack
November 20, 2025 AT 15:57Yash Nair
November 22, 2025 AT 06:02Bailey Sheppard
November 22, 2025 AT 12:50Heidi R
November 23, 2025 AT 04:08Brenda Kuter
November 24, 2025 AT 20:28Shaun Barratt
November 24, 2025 AT 23:13Girish Pai
November 26, 2025 AT 10:04Kristi Joy
November 26, 2025 AT 18:26Hal Nicholas
November 28, 2025 AT 15:28Louie Amour
November 29, 2025 AT 17:49Kristina Williams
December 1, 2025 AT 00:12