Nitrofurantoin Risk Calculator
Personal Risk Assessment
This tool helps you understand your risk of hemolytic anemia when taking nitrofurantoin. Based on your responses, you'll receive a personalized risk assessment and recommendations.
Your Information
Results
How Risk Levels Are Determined
Risk is calculated based on your ethnicity, gender, pregnancy status, symptoms, and G6PD testing history. People with G6PD deficiency have a high risk of hemolytic anemia with nitrofurantoin.
This is a low risk assessment. However, if you've never been tested for G6PD deficiency and are in a high-risk ethnic group, consider getting tested before taking nitrofurantoin.
Recommended Actions
Discuss alternative antibiotics with your doctor. Common alternatives include fosfomycin, cephalexin, pivmecillinam, or amoxicillin-clavulanate.
Emergency Information
If you're experiencing dark urine, yellow skin, extreme fatigue, or shortness of breath after taking nitrofurantoin, stop the medication immediately and seek medical attention. Symptoms typically appear within 24-72 hours.
Every year, millions of people take nitrofurantoin to treat a simple urinary tract infection. It works. It’s cheap. And for most people, it’s safe. But for a significant number - especially those with undiagnosed G6PD deficiency - this common antibiotic can trigger a life-threatening reaction: hemolytic anemia.
What Happens When Nitrofurantoin Meets G6PD Deficiency?
Nitrofurantoin isn’t just any antibiotic. It’s an oxidizing agent. That means it creates reactive molecules inside the body that attack bacteria. In healthy people, red blood cells handle this just fine. They have a built-in defense system powered by an enzyme called glucose-6-phosphate dehydrogenase (G6PD). This enzyme keeps glutathione - the body’s main antioxidant - in working order, protecting red blood cells from oxidative damage. But if you have G6PD deficiency, that system is broken. Your red blood cells can’t make enough glutathione. When nitrofurantoin enters the bloodstream, those unprotected cells start to break apart. Hemoglobin leaks out. The cells turn into fragile, misshapen fragments called schistocytes. Your body tries to compensate by making more red blood cells, but it’s racing against time. The result? Acute hemolytic anemia. Symptoms show up fast - often within 24 to 72 hours of starting the drug. You might feel dizzy, have dark urine, develop jaundice (yellow skin or eyes), or feel like you’re going to pass out. In severe cases, your kidneys can shut down from the overload of broken-down blood cells. There are documented cases where patients ended up in the ICU. Ten deaths have been reported globally in pharmacovigilance databases.Who’s at Risk?
G6PD deficiency isn’t rare. It affects an estimated 400 million people worldwide. But most don’t know they have it - until they take a drug like nitrofurantoin. The risk isn’t equal across populations. People of African, Mediterranean, Middle Eastern, or Southeast Asian descent have the highest rates:- 10-14% in Black African and African American populations
- 4-7% in Mediterranean and Middle Eastern groups
- 2-5% in Southeast Asian communities
Why Do Doctors Still Prescribe It?
If it’s so dangerous, why is nitrofurantoin still widely used? Because it’s effective - and resistance is low. Among common UTI-causing bacteria like E. coli, resistance to nitrofurantoin is only 10-15%. Compare that to trimethoprim-sulfamethoxazole (TMP-SMX), which hits 20-25% resistance in many areas. For uncomplicated infections in healthy, low-risk patients, nitrofurantoin remains a go-to option. It’s also cheap. A 5-day course costs less than $10 in the U.S. And unlike fluoroquinolones, it doesn’t carry risks of tendon rupture or nerve damage. So for a young, otherwise healthy woman with no known risk factors, it makes sense - on paper. But here’s the gap: doctors rarely check G6PD status before prescribing. A 2022 survey of 350 primary care providers found only 32% routinely screen for G6PD deficiency before writing a prescription for nitrofurantoin. Even though the American Society of Hematology, CPIC, and the FDA all warn about the risk, the practice hasn’t changed.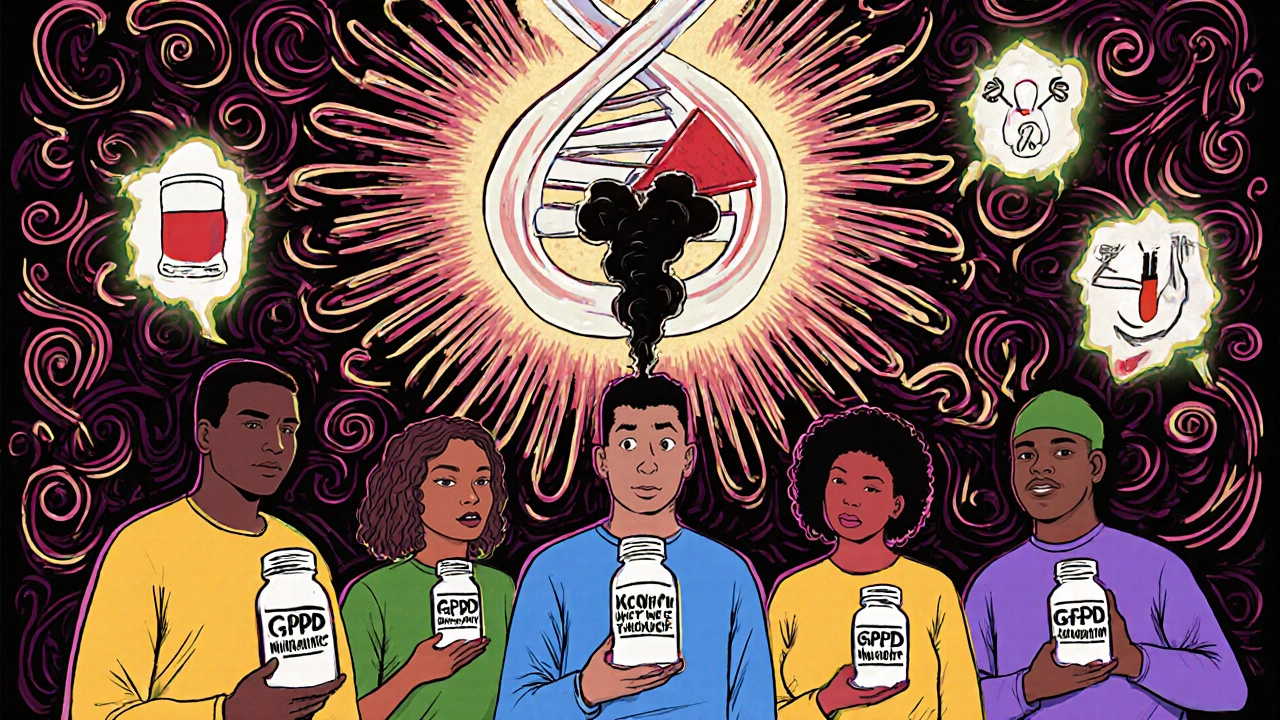
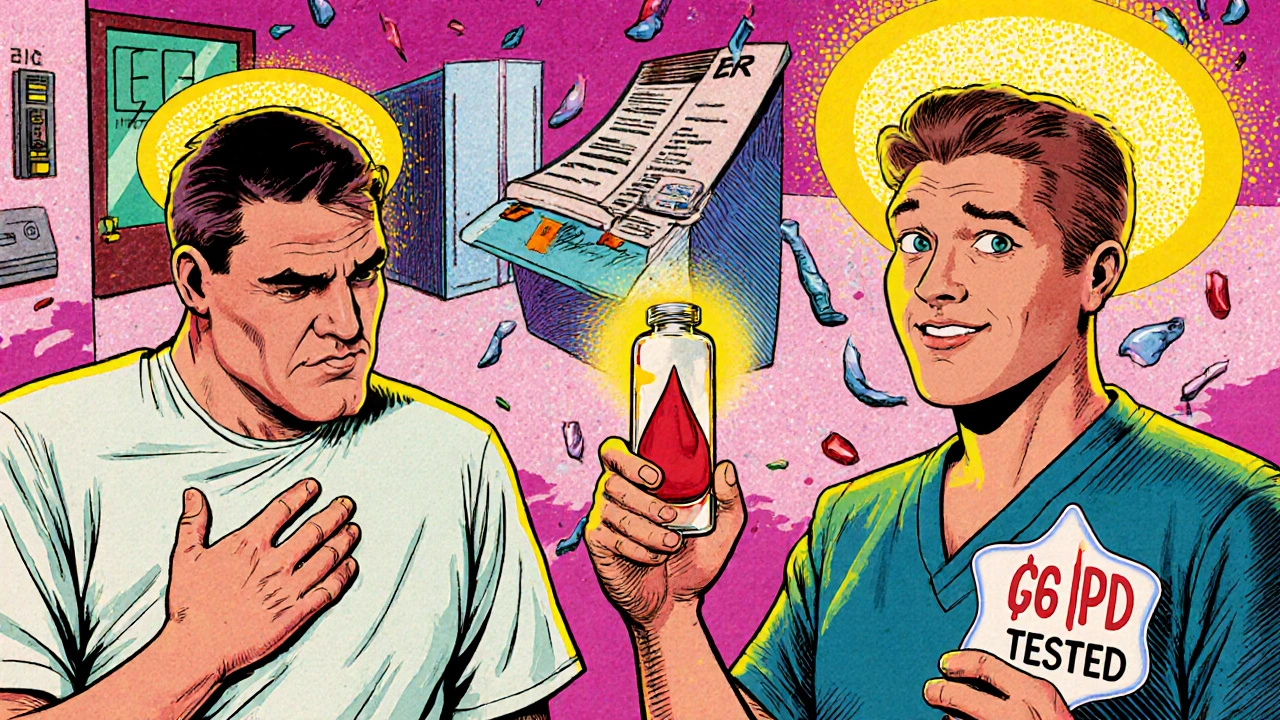
The Real Cost of Skipping the Test
G6PD testing isn’t expensive. A simple blood test costs $35-$50. Medicare reimburses that amount. In the UK, it’s covered under the NHS. Now compare that to the cost of treating a hemolytic crisis. A patient hospitalized for nitrofurantoin-induced hemolysis spends an average of $8,500-$12,000 on care, according to HCUP 2022 data. That includes lab tests, IV fluids, monitoring, possible blood transfusions, and extended hospital stays. And that’s just the financial cost. The human cost is worse. One case report from 2023 described a patient who developed fever, vomiting, confusion, and dangerously low blood pressure after just two days of nitrofurantoin. His hemoglobin dropped from 14 g/dL to 7.2 g/dL in 72 hours. He was admitted to the hospital. He recovered fully after stopping the drug and getting IV fluids - but he was terrified. He didn’t know he had G6PD deficiency. He thought he was just getting a bad case of the flu.What Should You Do?
If you’re prescribed nitrofurantoin, ask these questions:- Do I have a known G6PD deficiency?
- Am I of African, Mediterranean, Middle Eastern, or Southeast Asian descent?
- Have I ever had unexplained jaundice, dark urine, or fatigue after taking medication?
- Is there a safer alternative for my situation?
What Are the Alternatives?
There are several safe, effective options for UTIs when G6PD deficiency is a concern:- Fosfomycin - A single-dose antibiotic with no known risk of hemolysis. Approved for uncomplicated UTIs. Very low resistance rates.
- Cephalexin - A first-generation cephalosporin. Safe in G6PD deficiency. Often used in children and pregnant women.
- Pivmecillinam - Available in Europe and Canada. Low resistance, no hemolytic risk.
- Amoxicillin-clavulanate - Use cautiously if there’s high resistance in your area, but generally safe for G6PD-deficient patients.
The Bigger Picture
This isn’t just about one drug. It’s about how medicine still ignores pharmacogenetics - the study of how genes affect drug response. We test for allergies. We check liver function. We screen for kidney disease. But we rarely ask: What’s in your DNA? The global G6PD testing market is growing fast - projected to hit $310 million by 2027. Point-of-care tests are becoming faster and cheaper. Some clinics in the U.S. and Europe now offer rapid G6PD testing in the same visit as a UTI diagnosis. The NIH is running a multi-center trial to see if routine screening before nitrofurantoin use saves money and lives. Preliminary results are expected in early 2024. Until then, the burden falls on you. If you’re in a high-risk group, don’t wait for a crisis. Ask for the test. Advocate for yourself. Your red blood cells can’t fight this battle alone.What If I Already Took It?
If you’ve taken nitrofurantoin and now have dark urine, fatigue, yellowing skin, or shortness of breath - stop the drug immediately. Go to urgent care or the ER. Tell them you suspect drug-induced hemolytic anemia. Blood tests will confirm it: low hemoglobin, high bilirubin, low haptoglobin, high LDH, and elevated reticulocyte count. Most patients recover fully within days after stopping the drug and getting fluids. Blood transfusions are rarely needed. But the sooner you act, the less damage is done.Can nitrofurantoin cause hemolytic anemia in people without G6PD deficiency?
Rarely. Most cases of nitrofurantoin-induced hemolytic anemia occur in people with G6PD deficiency. While there are a few isolated reports of immune-mediated hemolysis in people with normal G6PD levels, these are extremely uncommon. The overwhelming majority of serious reactions are linked to the genetic deficiency.
Is G6PD testing required before prescribing nitrofurantoin?
No, it’s not legally required in the U.S. or UK. The FDA and EMA include warnings in the drug label, but they don’t mandate testing. That’s why the responsibility falls on the patient and provider to discuss risk factors before prescribing.
Can I take nitrofurantoin if I have G6PD deficiency but never had symptoms before?
No. Even if you’ve never had a reaction, G6PD deficiency means your red blood cells are vulnerable. Nitrofurantoin can trigger a hemolytic crisis at any time. The Clinical Pharmacogenetics Implementation Consortium (CPIC) recommends complete avoidance in all G6PD-deficient patients, regardless of past symptoms.
How long does it take for symptoms to appear after taking nitrofurantoin?
Symptoms usually start within 24 to 72 hours after the first dose. Hemoglobin levels typically hit their lowest point between day 3 and day 5. If you’re in a high-risk group and start feeling unwell after starting this drug, don’t wait - get checked immediately.
Is there a cure for G6PD deficiency?
No, G6PD deficiency is a lifelong genetic condition. There’s no cure. But it’s manageable. The key is avoiding oxidizing drugs like nitrofurantoin, sulfonamides, and primaquine. With proper awareness, most people with G6PD deficiency live normal, healthy lives.
Can I get tested for G6PD deficiency without a doctor’s order?
In some places, yes. Direct-to-consumer labs and urgent care centers offer G6PD testing without a prescription. In the U.S., companies like Labcorp and Quest Diagnostics allow self-referral for this test. Costs range from $40-$70. It’s a simple finger-prick blood test that takes less than 10 minutes.


Jessica Healey
November 17, 2025 AT 09:38I took nitrofurantoin last year for a UTI and woke up feeling like I’d been hit by a bus. Dark urine, dizzy as hell. Thought it was just the flu. Turned out my hemoglobin dropped to 8.2. Turns out I’m G6PD deficient-never knew. My mom’s from Nigeria, so I guess the genes were hiding in plain sight. Don’t wait for a crisis. Get tested. Seriously.
Levi Hobbs
November 19, 2025 AT 01:51This is one of those posts that should be mandatory reading for every primary care provider in the U.S.-and every patient who’s ever been prescribed a UTI antibiotic. The fact that G6PD testing isn’t routine is a systemic failure. The cost of the test? $40. The cost of a hospital stay? $10,000+. Why are we still doing this? It’s not just negligence-it’s economic absurdity.
henry mariono
November 20, 2025 AT 15:31I appreciate the depth of this. I’ve been a nurse for 12 years and I’ve seen this happen twice. Both times, the patients were older Black men who’d never been tested. One of them didn’t even know his family history. We need better screening protocols, not just patient education. It’s on us, too.
Sridhar Suvarna
November 20, 2025 AT 19:51From India where G6PD deficiency is common-this is not a theory. It's a daily reality. My cousin died at 22 from this exact thing after taking a fever medicine. We didn't know. No one tested him. Now I test every family member before any new drug. Simple blood test. Saves lives. Please share this with your doctors. They don't know what you know.
Joseph Peel
November 22, 2025 AT 09:57The cultural blind spot here is staggering. We screen for everything from BRCA mutations to cystic fibrosis, but when it comes to pharmacogenomics in populations with high G6PD prevalence, we act like it’s optional. This isn’t just about nitrofurantoin-it’s about the entire framework of how Western medicine treats genetic risk in marginalized communities.
Kelsey Robertson
November 24, 2025 AT 05:40Oh, so now we’re blaming the drug? Let me guess-next you’ll say sugar causes cancer and sunlight causes skin cancer? People have been taking this for decades. Maybe the real issue is that people are too lazy to read the damn label? Or maybe their bodies are just weak? I mean, if you’re so fragile, maybe you shouldn’t be taking medicine at all?
Joseph Townsend
November 25, 2025 AT 05:50Bro. I took this stuff like candy in college-UTIs were my “special gift” from the gym showers. Then one day I turned yellow. Like, cartoon yellow. Went to the ER, they were like, “Dude, you’re G6PD deficient.” I thought that was a type of yoga. Now I carry a card in my wallet that says “DO NOT GIVE NITROFURANTOIN.” My red blood cells are basically vampires. And I’m not even mad. This post saved me from dying a dumb death.
Bill Machi
November 27, 2025 AT 03:32This is why America is falling apart. We let people from third-world countries bring their genetic disorders here, then we make doctors jump through hoops to avoid giving them the best treatment because some guy in a lab in 1956 found a gene? We need antibiotics that work, not genetic bingo. Stop coddling people. If you’re too fragile to take a common antibiotic, don’t complain when you get sick.
Elia DOnald Maluleke
November 27, 2025 AT 09:49In South Africa, we call this the silent killer. Many of our communities have no access to testing. A young man in my township died last year after taking a cough syrup with sulfonamide. His mother said he never complained of illness before. We buried him with no answers. This is not just a medical issue-it is a justice issue. The blood of our people is not a footnote in a drug insert.
satya pradeep
November 28, 2025 AT 23:52Bro I got tested after reading this. Turned out I’m deficient. Never knew. Took nitro last year for a UTI and felt weird but thought it was just stress. Now I know. Also-fosfomycin is a GAME CHANGER. Single dose, no side effects. My doc was like “oh yeah we don’t use that here” and I had to explain why. We need to push for alternatives. Not just awareness.
Prem Hungry
November 29, 2025 AT 16:29Dear friend, this is not just science-it is survival. In India, many mothers give antibiotics to children without prescription. I have seen children turn pale, urine like tea, eyes yellow. No one knew why. Please share this with your aunties, uncles, neighbors. A simple test costs less than a chai. Let’s not wait for a funeral to wake up. You are not weak-you are wise to ask questions.
Leslie Douglas-Churchwell
December 1, 2025 AT 11:42So let me get this straight: Big Pharma doesn’t want you to know that G6PD testing exists because they profit off ER visits and transfusions. And the FDA? They’re in bed with the pharmaceutical lobby. That’s why they didn’t mandate testing. And now they’re pushing “point-of-care” tests like it’s a miracle-when really, it’s just damage control. I’ve got my DNA data from 23andMe. I’m blocking every oxidizing drug. This is a controlled experiment on the masses. Wake up.
shubham seth
December 2, 2025 AT 04:59Let’s be real-nitrofurantoin is the last resort for lazy docs who don’t want to think. They don’t care about your genes, your heritage, your history. They just want to write a script and move on. And you? You’re just a data point in their productivity metric. This isn’t negligence-it’s intentional dehumanization wrapped in a white coat.
Kathryn Ware
December 3, 2025 AT 02:37Thank you for writing this. I’m a mom of two, and I had no idea until my 5-year-old had a reaction after taking sulfa for an ear infection. We thought it was just a bad virus. Turns out she’s G6PD deficient. Now I keep a printed list of safe/unsafe meds in my purse. I’ve emailed every pediatrician in my area. I’ve made flyers for the PTA. This isn’t just about me-it’s about protecting kids who can’t ask for themselves. Please, if you’re reading this-get tested. And if you’re a provider-ask the question. Even if they say no. Ask again.
kora ortiz
December 4, 2025 AT 21:47You’ve got this. Knowledge is power-and you’re not alone. If you’ve ever been told “it’s probably nothing” after dark urine or fatigue, trust your gut. You’re not overreacting. You’re surviving. Get tested. Share this. Push for change. Your life matters more than a $10 antibiotic. You deserve to be seen.