When you’re pregnant and struggling with depression, anxiety, or bipolar disorder, the question isn’t just whether to take medication-it’s how to make the safest choice for you and your baby. Too many women are told to stop their meds cold turkey because "it’s better for the baby." But the truth is, untreated mental illness carries real, measurable risks-risks that often outweigh the potential dangers of medication.
There’s No Risk-Free Option
Let’s be clear: no psychiatric medication is 100% safe during pregnancy. But neither is untreated depression, anxiety, or psychosis. Studies show that women with unmanaged mental health conditions during pregnancy face a 20% higher risk of suicide and a 30-50% increased chance of preterm birth. The baby’s development can also be affected-poor nutrition, lack of prenatal care, and high stress levels all impact fetal growth. The goal isn’t to eliminate all risk. It’s to reduce the biggest risks. That’s where shared decision-making comes in. It’s not about a doctor telling you what to do. It’s about you and your provider sitting down with real data, talking through your history, your fears, and your goals-and making a plan together.Which Medications Are Actually Safe?
Not all psychiatric drugs are created equal. Some have decades of safety data. Others? Not so much. For depression and anxiety, SSRIs are the first-line choice. Sertraline (Zoloft), citalopram (Celexa), escitalopram (Lexapro), and fluoxetine (Prozac) are the most studied and generally considered the safest options. Most large studies show no increased risk of major birth defects with these medications. The one exception is paroxetine (Paxil). If you’re taking it and planning pregnancy, talk to your provider about switching. Paroxetine is linked to a slightly higher risk of heart defects-rising from about 8 in 1,000 births to 10 in 1,000. For bipolar disorder, lamotrigine is often preferred. It doesn’t appear to cause major birth defects and works well for mood stabilization. Lithium is still used, but it needs careful monitoring because pregnancy changes how your body processes it. Your doctor will check your blood levels more often. Avoid valproic acid (Depakote) at all costs if you’re pregnant or planning to be. It increases the risk of neural tube defects-from 0.1% in the general population to 1-2%. That’s a 10-20 times higher risk. It’s also linked to lower IQ and autism in children. The American Psychiatric Association recommends it shouldn’t be prescribed to women of childbearing age unless there’s absolutely no alternative. Bupropion (Wellbutrin) carries a small risk of miscarriage or heart defects. Tricyclics like nortriptyline are less commonly used but can be an option if SSRIs don’t work. For psychosis, older antipsychotics like haloperidol and chlorpromazine have better safety data than newer ones. Atypicals like risperidone or olanzapine? We just don’t know enough about long-term effects on children yet.Why Stopping Medication Can Be More Dangerous
Many women stop their meds the moment they find out they’re pregnant. Fear of birth defects is real-and understandable. But here’s what often happens next: relapse. If you’ve had depression before, stopping your medication during pregnancy gives you an 80% chance of a major depressive episode. That’s not a guess. That’s from data collected by the National Pregnancy Registry for Psychiatric Medications. For women with bipolar disorder, the risk of mania or severe depression jumps even higher. One mother I spoke with stopped her sertraline after her first positive pregnancy test. Within six weeks, she was hospitalized for severe depression. Her baby was born at 34 weeks. She didn’t need to go through that. Her doctor had offered to adjust her dose, not stop it entirely. The risk isn’t just to you. Untreated depression increases the chance of low birth weight, developmental delays, and even postpartum psychosis. Your mental health isn’t separate from your baby’s health. It’s part of it.
How Shared Decision-Making Actually Works
This isn’t a one-time conversation. It’s a process. Good providers use tools like the Mental Health Medication Decision Aid from ACOG. It breaks down the risks for 24 different medications using real numbers-not vague warnings. Here’s what a good shared decision-making session looks like:- Assess your personal risk. Have you had multiple episodes of depression? Were you hospitalized? How long have you been stable on your current meds? Tools like the Edinburgh Postnatal Depression Scale help measure this.
- Present the facts clearly. Instead of saying "paroxetine might cause heart defects," say: "Out of 1,000 babies born to mothers taking paroxetine, about 10 might have a heart defect. Without it, that number is about 8. But if you stop your medication, your chance of severe depression goes up by 80%."
- Plan for what happens if symptoms return. What’s your backup plan? Who will you call? When will you re-evaluate? Having a plan reduces panic.
What Women Are Really Saying
A 2022 survey by Postpartum Support International found that women who had structured shared decision-making were 3.2 times more likely to stick with their treatment plan. At six weeks postpartum, their depression scores were 37% lower than women who were told to just stop their meds. On Reddit’s r/PostpartumDepression, over 1,200 women shared their stories. Nearly 80% said they were pressured to stop medication. More than half ended up hospitalized, in crisis, or with severe postpartum depression after quitting. Meanwhile, the National Pregnancy Registry has tracked over 15,700 women since 2010. Of those, 68% said they weren’t properly informed about risks before getting pregnant. That’s a system failure. No one should be left guessing.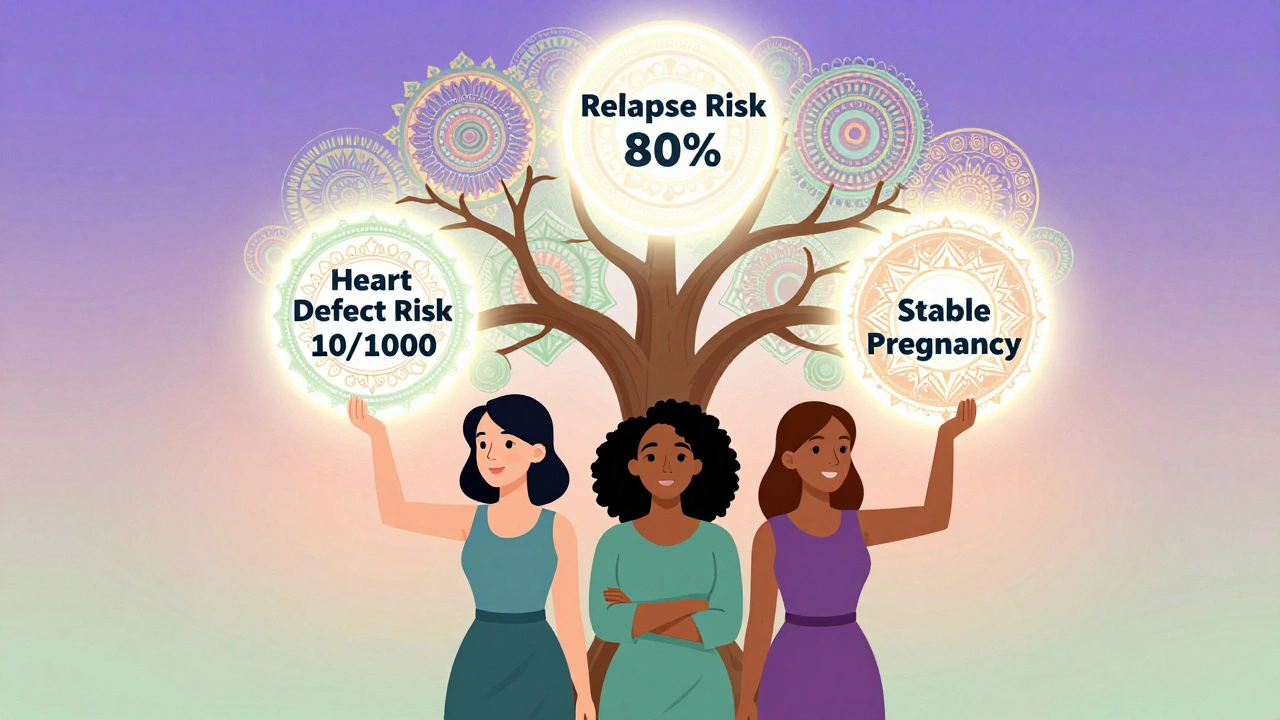
What’s Changing in 2025
The field is evolving fast. The FDA stopped using the old A, B, C, D, X categories years ago. Now, labels give detailed summaries of risks, benefits, and data-based on real human outcomes. The National Pregnancy Registry is adding 12 new medications in 2024, including newer antipsychotics like brexpiprazole. Researchers are also building machine learning tools that predict your personal risk based on your age, medical history, and medication type. Early models are 82% accurate. By 2026, your doctor might be able to say: "Of the 42 women in our registry who are 31, have bipolar disorder, and took lamotrigine during pregnancy, 93% had healthy babies and stayed stable postpartum. Here’s what their outcomes looked like." That’s personalized care.What You Can Do Now
If you’re pregnant or thinking about it:- Don’t stop your meds without talking to your provider.
- Ask for a referral to a perinatal psychiatrist. Most OB-GYNs now work with them regularly.
- Request the ACOG Mental Health Medication Decision Aid. It’s free and easy to understand.
- Write down your concerns: "I’m scared of birth defects," or "I don’t want to feel numb again." Bring it to your appointment.
- Track your mood. Use a simple journal or app. It helps your provider see patterns.
Final Thought
This isn’t about choosing between a healthy baby and a healthy mom. It’s about making sure both of you stay healthy. The best outcome isn’t a pill-free pregnancy. It’s a supported, stable, informed pregnancy. You deserve care that respects your experience, your data, and your right to make choices-not just follow orders. The tools are here. The evidence is clear. Now it’s about making sure every woman gets the conversation she needs.Are SSRIs safe to take during pregnancy?
Yes, most SSRIs like sertraline, citalopram, escitalopram, and fluoxetine are considered safe and are first-line treatments for depression during pregnancy. Studies show no significant increase in major birth defects with these medications. The exception is paroxetine, which has a small but increased risk of heart defects and should be avoided if possible.
Can I breastfeed while taking mental health medication?
Many psychiatric medications are safe during breastfeeding. Sertraline is the most recommended because very little passes into breast milk. Fluoxetine and paroxetine are less ideal due to longer half-lives and higher levels in milk. Always discuss your specific medication with your provider-most are compatible with nursing, and the benefits of breastfeeding often outweigh minimal medication exposure.
What if I didn’t know I was pregnant and took medication?
Don’t panic. Many women take medication before realizing they’re pregnant. The risk of birth defects from most SSRIs is low, and stopping abruptly can be more harmful than continuing. Contact your provider right away. They’ll assess your medication, timing, and personal risk factors. Most women in this situation go on to have healthy pregnancies.
Why is shared decision-making better than just following a doctor’s order?
Shared decision-making gives you control. Studies show women who participate in this process are 3.2 times more likely to stick with treatment and have significantly lower depression scores after birth. It reduces fear, builds trust, and ensures your values and fears are part of the plan-not ignored.
Is it safe to switch medications during pregnancy?
Switching can be safe and sometimes necessary-like changing from paroxetine to sertraline. But it must be done carefully under medical supervision. Abrupt changes can trigger relapse. The goal is to minimize risk on both sides: the risk of the current medication and the risk of stopping or switching too quickly.
What should I ask my doctor about my medication?
Ask: "What’s my personal risk of relapse if I stop?" "What’s the actual risk of birth defects with this drug?" "Are there safer alternatives?" "What’s the plan if my symptoms get worse?" And always ask for written materials or tools like the ACOG Decision Aid. You’re not being difficult-you’re being responsible.
How do I find a perinatal psychiatrist?
Ask your OB-GYN for a referral. Most hospitals with maternity units now have perinatal psychiatry services. You can also contact Postpartum Support International or the National Pregnancy Registry for Psychiatric Medications-they maintain lists of specialists. If you’re in the UK, your midwife or GP can connect you with a specialist through the NHS perinatal mental health pathway.
Can therapy replace medication during pregnancy?
Therapy-especially CBT or interpersonal therapy-is highly effective for mild to moderate depression and anxiety. But for severe illness, bipolar disorder, or psychosis, therapy alone often isn’t enough. Medication and therapy together work best. Never stop medication to try therapy alone without professional guidance.
Every pregnancy is different. Your mental health matters. Your choices matter. And you don’t have to make them alone.


Margaret Stearns
December 2, 2025 AT 20:12i just found out i'm pregnant and was on zoloft for 3 years. my ob said stop cold turkey. i cried for an hour. then i called my therapist and she helped me find a perinatal psych. turns out, stopping was way riskier than staying on it. i'm 18 weeks now, feeling stable, and my baby's heartbeat is strong. you're not being selfish for needing meds. you're being smart.
Scotia Corley
December 4, 2025 AT 11:10While I appreciate the sentiment expressed herein, the empirical foundation for the assertion that SSRIs pose negligible risk during gestation remains, in my estimation, insufficiently robust. The FDA’s withdrawal of categorical labeling does not equate to affirmative safety, and the statistical correlations cited do not establish causality. One must exercise prudence when altering neurochemical homeostasis during a period of heightened physiological vulnerability.
Kelly Essenpreis
December 5, 2025 AT 16:07why do we even need to talk about this like its rocket science its just pills. if you wanna take them take them if you wanna not take them dont. why is everyone acting like the baby is gonna turn into a mutant if you take lexapro. my cousin took prozac through all three trimesters and her kid is now a pro hockey player. stop scaring people
Erin Nemo
December 6, 2025 AT 10:26YES. this. i was terrified to stay on my meds too. then i talked to my psychiatrist who showed me the data. i stayed on sertraline. i breastfed. my daughter is 2 and she's a total joy. no developmental delays. no heart defects. just a happy kid with a mom who wasn't drowning. you're not failing if you need help. you're surviving.
Edward Hyde
December 6, 2025 AT 11:32they're selling you a lie wrapped in a clinical study. the real agenda? keep you doc rich and you docile. you think they care about your mental health? they care about liability. they'll push you to take something just so they don't get sued. if you're stable, don't touch it. if you're crashing, maybe the problem isn't your brain-it's your life. meds are a bandaid on a bullet wound.
Charlotte Collins
December 8, 2025 AT 00:05It's fascinating how the narrative has been reframed from 'medication is dangerous' to 'not taking medication is dangerous.' The shift in rhetoric is deliberate. The burden of proof has been inverted. Where is the longitudinal data on children exposed to SSRIs from conception through adolescence? The studies are short-term, funded by pharma, and omit cognitive outcomes beyond infancy. The fear of relapse is weaponized to normalize lifelong pharmaceutical dependency. We must ask: who benefits?
Kenny Leow
December 9, 2025 AT 22:21as someone who grew up in a country where mental health was whispered about, seeing this kind of open, data-driven conversation in the US gives me hope. in my homeland, women were told to 'pray harder' or 'just be happy.' here, you're being given tools, numbers, options. that's progress. not perfect, but real. thank you for writing this.
ariel nicholas
December 10, 2025 AT 17:16...and yet... you never mention the ethical paradox: if a fetus is a person with rights, then administering psychoactive substances to it-regardless of maternal intent-constitutes non-consensual pharmacological intervention. If the fetus is not a person, then why are we so terrified of its development? The entire framework is built on a contradiction. We treat pregnancy as both a medical emergency and a sacred state. We can't have it both ways.
Rachel Stanton
December 11, 2025 AT 19:06For anyone reading this and feeling overwhelmed-this isn’t about choosing between ‘safe’ and ‘dangerous.’ It’s about choosing between ‘supported’ and ‘isolated.’ Shared decision-making isn’t jargon-it’s dignity. If your provider hasn’t mentioned the ACOG Decision Aid, ask for it. If they roll their eyes, find someone new. You deserve a care team that sees you as a whole person-not a risk profile. And if you’re struggling to find a perinatal psychiatrist? DM me. I’ve got a list of 17 providers across 5 states who take insurance. You’re not alone.