Getting the right dose of medicine for a child isn’t just tricky-it’s life-or-death. A wrong number, a misread label, or a confused schedule can lead to serious harm. Unlike adults, kids don’t get standard doses. Their weight, age, and even developmental stage change how much medicine they need. One milligram too much can be dangerous. One milligram too little might not help at all. That’s why tracking pediatric doses isn’t optional-it’s essential.
Why Manual Dosing Is Risky
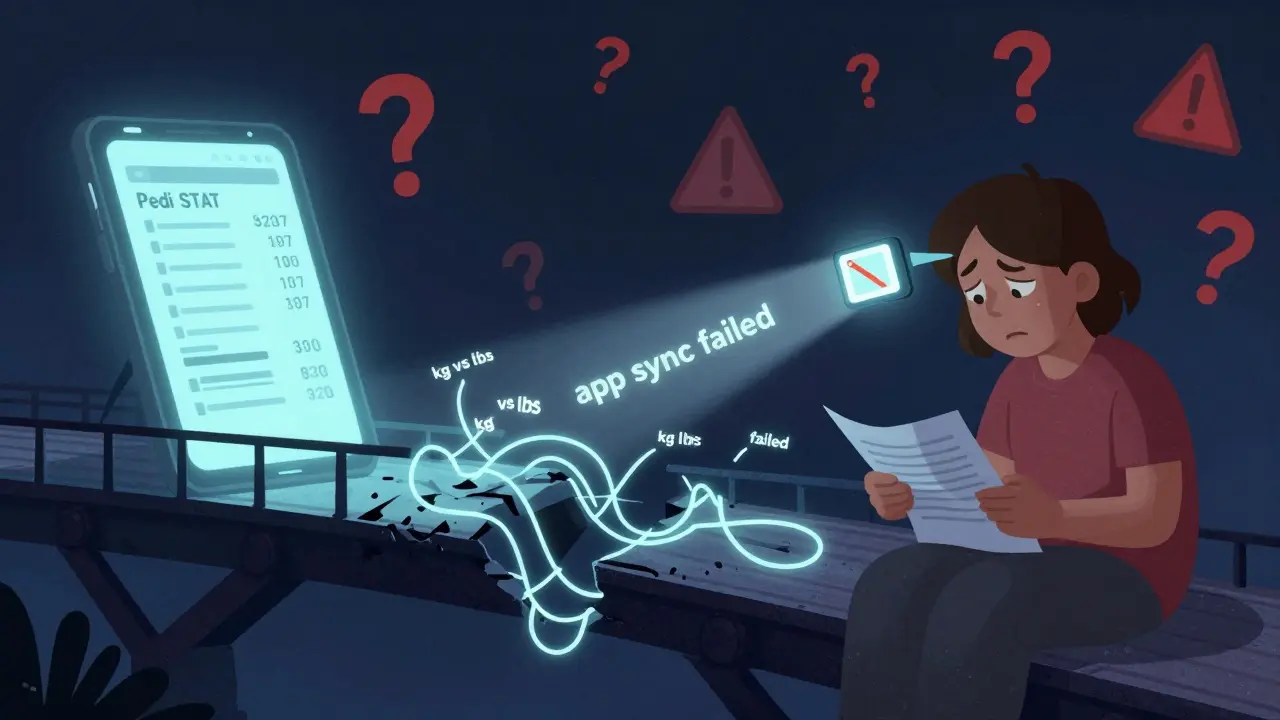
For years, doctors, nurses, and parents relied on paper charts, calculators, and memory to figure out how much medicine a child should get. But manual calculations are slow and error-prone. A 2022 study in Pediatric Emergency Care found that when clinicians calculated doses by hand, they made mistakes in over 12% of cases. That’s more than one in ten. In a real emergency, those seconds spent figuring out epinephrine or acetaminophen can cost precious time-and sometimes, a child’s life. Parents aren’t immune to these risks either. A 2023 survey by the American Academy of Pediatrics found that 87% of medication errors in children happened during transitions-like when a kid came home from the hospital. A parent might get a handwritten instruction saying "5 mL every 6 hours," but forget whether it’s for Tylenol or ibuprofen. Or they might misread the syringe. Or worse, they might enter the child’s weight in pounds instead of kilograms into a free app that doesn’t warn them. One documented case in the Journal of Pediatric Pharmacology and Therapeutics involved a 22-month-old who got 300% too much ibuprofen because of this exact mistake.Clinician Tools: Fast, Accurate, and Built for Emergencies
In hospitals and clinics, professionals rely on apps built for speed and precision. Pedi STAT is one of the most widely used. Developed by emergency doctors at Connecticut Children’s Medical Center back in 2009, it was designed for one thing: preventing deadly mistakes during urgent care. It lets you enter a child’s weight in kilograms (or pounds, with an auto-converter), and within three seconds, it gives you the correct dose for 15+ emergency medications-epinephrine, albuterol, antibiotics, you name it. It even suggests the right size of IV catheters and endotracheal tubes based on height. Another tool, Epocrates, has been around since 1998 and is used by over 1 million clinicians. It doesn’t just calculate doses-it checks for drug interactions across 35,000+ combinations. If a child is on antibiotics and a seizure medication, Epocrates will flag potential conflicts. The free version covers basic dosing, but the $175/year subscription adds advanced features like formulary checks and prescribing guidelines. These apps aren’t just convenient-they’re proven. A 2023 NIH study showed that using these tools cut calculation time by 67% and reduced dosing errors by 43% compared to paper methods. Dr. Robert Vinci from Boston Medical Center says mobile calculators have slashed critical errors in pediatric emergencies by 40-60% since 2015. But these tools have limits. They’re designed for professionals. Pedi STAT and Epocrates don’t sync with your home records. You can’t share a dose log from the hospital app to your phone at home. And they require training. A 2023 onboarding report from Connecticut Children’s found it takes about 2.3 hours for a new user to become proficient. That’s fine in a hospital, but useless for a tired parent at 2 a.m.Parent Apps: Simplicity, Reminders, and Safety Nets
For families, the goal isn’t to become pharmacists-it’s to avoid mistakes. That’s where apps like My Child’s Meds come in. Developed with input from the Royal College of Paediatrics and Child Health and WellChild, this app is built for caregivers. It lets you add each child’s medications with exact dosages, times, and reasons. You can set reminders for every dose. If you try to enter a second dose too soon, it warns you. It even lets you take a photo of the pill bottle and label it, so you know what’s what. One feature that stands out is its visual dose tracker. Instead of typing "5 mL," you tap a colored icon: green for given, red for missed, yellow for delayed. Parents report a 38% drop in dosing errors after using it. A verified user, Sarah K., wrote in her review: "This app saved us from a potential overdose when my toddler’s fever reducer schedule got confusing during night feedings." Another popular option is NP Peds MD, which gives you quick access to pediatrician-approved dosage tables for common over-the-counter meds like Tylenol, Motrin, and cough syrups. It doesn’t calculate-it just shows you the right amount based on weight. A 2024 Consumer Reports evaluation found that 78% of parents using this app gave the correct dose, compared to only 52% using printed charts. These apps are free or low-cost. My Child’s Meds costs nothing. NP Peds MD is free too. But they’re not perfect. They don’t connect to hospital systems. They can’t replace clinical judgment. And if you download a random app from the Google Play Store with no medical backing, you’re playing Russian roulette. One unvalidated app was linked to that 300% overdose case.
The Big Gap: When Hospital Meets Home
The biggest problem isn’t the apps-it’s the disconnect. A child leaves the hospital with a paper discharge sheet. The parent opens My Child’s Meds and tries to type in what the nurse said. But the nurse wrote "10 mg/kg" and the parent doesn’t know what that means. Or the hospital uses Pedi STAT, but the app doesn’t export data. The parent has to re-enter everything manually. A 2024 WellChild survey found that 68% of parents struggled to transfer medication info from hospital to home. That’s a massive gap. And it’s where most errors happen. Some hospitals are starting to fix this. ChildrensMD, a newer app, lets parents send a summary of their child’s meds directly to the provider’s portal. Early data shows this cuts information gaps by 57%. But it’s still rare. Most apps don’t talk to each other because of privacy rules (HIPAA) and technical barriers.What to Look for in a Pediatric Dose App
If you’re a parent, here’s what matters:- Is it clinically validated? Look for apps developed with pediatric hospitals or pharmacy groups. My Child’s Meds is endorsed by the Royal College of Paediatrics. Avoid apps with no medical backing.
- Does it prevent double dosing? The best apps block you from entering a dose too soon. That’s a lifesaver.
- Can you add photos of bottles? Visual labeling helps when you’re tired or stressed.
- Does it use kilograms? If the app asks for weight in pounds without auto-converting, be careful. Always double-check the unit.
- Is it free or low-cost? You don’t need to pay $70 for a dosing app. Stick to trusted free options.
- Use Pedi STAT for emergencies. It’s fast, accurate, and built for chaos.
- Use Epocrates for complex cases. Its drug interaction checker is unmatched.
- Always verify the output. Even the best app can glitch. Know how to calculate epinephrine manually-just in case.
- Recommend My Child’s Meds to families. It’s the only app parents need at home.
Best Practices to Avoid Mistakes
No app is foolproof. Here’s how to stay safe:- Always confirm the weight unit. Kilograms, not pounds. If you’re unsure, ask.
- Double-check with a second source. Cross-reference the app’s dose with the Harriet Lane Handbook or a printed chart.
- Keep a paper backup. Power outages happen. Phones die. Always have a printed dosing schedule.
- Reconcile weekly with your pharmacy. Children’s Hospital of Philadelphia recommends this. Your pharmacist can catch mismatches.
- Train everyone who gives meds. Grandparents, babysitters, siblings-make sure they know how to use the app or read the chart.
What’s Next?
The future is coming fast. Pedi STAT is testing AI that predicts when a dose is likely to be wrong before it’s given. Boston Children’s Hospital is trialing smart pill dispensers that unlock only at the right time. And HIMSS is working on a new data standard to let hospital apps talk to parent apps-expected by late 2025. By 2027, experts predict 95% of pediatric doses in hospitals will be digitally verified. That’s huge. But for families, the goal is simpler: one less sleepless night worrying about whether they gave the right amount.Can I use any medication app for my child?
No. Only use apps developed with medical input, like My Child’s Meds or NP Peds MD. Avoid random apps from the app store-they may not be accurate or safe. Check if the app is endorsed by a children’s hospital or pediatric pharmacy group.
Do pediatric dosing apps replace the need to know how to calculate doses manually?
No. While apps reduce errors, relying on them completely is dangerous. A 2023 simulation study found 22% of medical residents couldn’t calculate an epinephrine dose when their device failed. Always learn the basic formulas and keep a paper backup.
What’s the difference between Pedi STAT and My Child’s Meds?
Pedi STAT is for healthcare providers in emergencies-it calculates doses for critical meds in seconds. My Child’s Meds is for parents at home-it tracks schedules, sends reminders, and prevents double dosing. They serve different roles and don’t connect.
Are free pediatric dosing apps safe?
Some are, some aren’t. Free apps like NP Peds MD and My Child’s Meds are safe because they’re backed by medical experts. But many free apps on Google Play are just pill organizers with no dosing logic. Always check the developer and look for clinical endorsements.
How do I know if my child’s dose is correct?
Compare the app’s recommendation with the prescription label and a trusted reference like the Harriet Lane Handbook. If there’s any doubt, call your pharmacist or pediatrician. Never guess. Even a small error can be dangerous in children.


Liz MENDOZA
December 27, 2025 AT 13:11As a pediatric nurse and mom of two, I’ve seen too many parents panic because they’re unsure if they gave the right dose. My Child’s Meds wasn’t just helpful-it was a lifeline during that week my son had the flu and we were juggling three different meds. The photo-label feature? Genius. I snapped pics of every bottle and labeled them ‘Tylenol - 10mg/kg’ so even my husband could use it at 3 a.m. No more guessing.
And yes, paper backups are non-negotiable. I keep a laminated card in my wallet with the emergency doses for epinephrine and ibuprofen. Phones die. Batteries drain. But paper? It’s always there.
Miriam Piro
December 28, 2025 AT 16:29Let’s be real-this whole ‘app safety’ narrative is just corporate propaganda wrapped in pediatric jargon. 😒
Who’s really behind these ‘clinically validated’ apps? Big Pharma. They fund the studies, they design the interfaces, they even pay the ‘experts’ who endorse them. The 300% overdose case? That wasn’t the app’s fault-it was the hospital’s failure to standardize protocols. And now they want us to trust another app? HA.
Meanwhile, the real issue is that pediatric dosing is still based on weight, not metabolic rate, which varies wildly by ethnicity, nutrition, and even gut microbiome. But nope-let’s just stick to the same outdated kg-based formulas and slap a ‘safe’ sticker on it. 🤡
And don’t get me started on HIPAA blocking interoperability. That’s not privacy-it’s profit. Hospitals don’t want your data flowing to parent apps because then they’d lose control. It’s not about safety. It’s about power.
My advice? Learn the math. Memorize the formulas. Trust your gut. And delete every app that asks for your child’s weight. You’re not a data point.
They’re selling peace of mind. But real safety? That’s free. And it’s called knowledge.
Nikki Thames
December 28, 2025 AT 16:59While I appreciate the clinical rigor presented here, I must emphasize that the foundational assumption-that technological intervention can supplant clinical judgment-is both empirically unsound and ethically precarious. The reliance on digital tools fosters a dangerous epistemic dependency, wherein the caregiver abdicates cognitive responsibility to algorithmic outputs. This is not innovation; it is institutionalized complacency.
Furthermore, the normalization of mobile applications in pediatric pharmacotherapy obscures the deeper structural failures of healthcare delivery: fragmented care coordination, inadequate provider training, and the commodification of parental anxiety. One cannot ‘solve’ systemic dysfunction with a 99-cent app.
One must ask: Who benefits from this digitization? The parent? The clinician? Or the app developer, whose revenue model is predicated on perpetual engagement and data extraction?
True safety lies not in the interface, but in the cultivation of clinical literacy, interprofessional communication, and the restoration of the human element in care. The algorithm cannot grieve when a child dies. But a nurse can.
And so I ask: Are we healing children-or optimizing user retention metrics?
Todd Scott
December 30, 2025 AT 13:06Just came back from a trip to Nigeria with my niece-she was on antibiotics after a bout of pneumonia. We had zero access to apps, no internet, no hospital records. But we had the Harriet Lane Handbook, a small printed dosing chart, and a local pharmacist who spoke both English and Yoruba.
Here’s the thing: in places where tech is unreliable, human knowledge becomes the real safety net. The apps are great for the US, sure. But let’s not pretend they’re universal. In rural India, rural Nigeria, rural Appalachia-people are still using paper, memory, and community wisdom.
And honestly? That’s not a flaw. That’s resilience.
What we need isn’t just better apps-it’s better training for caregivers everywhere. Teach them how to read a syringe. Teach them to ask, ‘Is this in kg or lbs?’ Teach them to say, ‘I’m not sure, let me call someone.’
Technology should augment, not replace, that human instinct.
Also-NP Peds MD? Free? Yes. And it saved my niece’s life. No hype. Just facts.
Andrew Gurung
December 31, 2025 AT 10:54Let me just say-this entire post reads like a pharmaceutical ad written by someone who’s never held a crying toddler at 2 a.m.
My Child’s Meds? Cute. But when your kid is feverish, you’re not tapping colored icons. You’re holding their head, wiping their forehead, and Googling ‘is 10mL of Tylenol too much for 22 lbs?’ while your partner yells, ‘WHICH BOTTLE IS WHICH?!’
And don’t get me started on ‘clinically validated’-that’s just corporate-speak for ‘we paid a doctor to say yes.’
Meanwhile, the real MVP? The nurse who scribbled ‘5 mL every 6 hrs - Tylenol - NOT Motrin’ on a napkin and taped it to the fridge. No app. No sync. No login. Just ink.
Also, Epocrates? $175/year? Are you kidding me? My resident gets it for free because she’s a ‘professional.’ Meanwhile, I’m paying $15/month for a fitness app that tells me to ‘drink more water.’
System is rigged. And we’re just the guinea pigs.
Paula Alencar
January 2, 2026 AT 06:32The emotional weight of this topic cannot be overstated. As a mother of a child with complex medical needs, I have lived the terror of a missed dose, the guilt of a double dose, the paralyzing fear that I, a non-professional, am holding the fate of my child’s life in my trembling hands.
My Child’s Meds did not just organize my daughter’s regimen-it restored my dignity. For the first time, I felt like a competent caregiver, not a terrified amateur. The visual tracker? It gave me back sleep. The reminder tones? They became the soundtrack of my survival.
But let us not mistake convenience for cure. The true tragedy is that this tool exists only because our healthcare system has failed to provide continuity. Why must a parent become a pharmacist? Why must a mother memorize weight-based formulas when the hospital could simply send a digital summary to her phone?
Until interoperability becomes a human right-not a HIPAA loophole-we are merely bandaging a wound that needs surgery.
I am grateful for the app. But I am furious that it was ever necessary.
Chris Garcia
January 3, 2026 AT 10:44Interesting how we treat pediatric dosing like a math problem, when it’s fundamentally a cultural one.
In my village in Nigeria, we never used apps or charts. We used the ‘hand method’-a pinch for powders, a thumb’s width for syrups, a teaspoon from the kitchen. We trusted elders, we observed outcomes, we adjusted based on how the child looked-not how the scale read.
Now, we import Western apps and call them ‘safe’-but they’re built for a world that doesn’t exist for most. What if your scale only measures in stones? What if your child weighs ‘about the same as a sack of yams’? What if you can’t afford a phone with GPS?
Technology doesn’t solve inequality. It amplifies it.
Maybe the real innovation isn’t an app that calculates-but a system that respects. That listens. That trusts the mother who’s been doing this for years, even if she can’t read the label.
Knowledge isn’t always digital. Sometimes, it’s whispered from grandmother to mother, passed down like a secret prayer.
James Bowers
January 5, 2026 AT 04:05The author’s uncritical endorsement of proprietary medical software is both irresponsible and deeply misleading. The notion that a mobile application-designed by for-profit entities with no fiduciary duty to patient safety-can reliably supplant clinical expertise is not merely optimistic; it is dangerously naive.
Furthermore, the claim that ‘free apps are safe’ is a fallacy. Free does not mean validated. Free does not mean audited. Free does not mean free from hidden data harvesting. The proliferation of unregulated medical apps constitutes a public health threat of alarming proportions.
Moreover, the suggestion that parents should rely on ‘My Child’s Meds’ while ignoring the fundamental requirement of pharmacological literacy is a dereliction of professional responsibility. No algorithm can replace the critical thinking required to interpret a prescription, verify a unit, or recognize a contradiction.
There is no substitute for education. There is no shortcut for vigilance. And there is no moral justification for outsourcing life-or-death decisions to a smartphone.
Will Neitzer
January 5, 2026 AT 22:29I’ve been a pediatric pharmacist for 18 years, and I can tell you-this post nails it. The disconnect between hospital and home is the silent killer in pediatric care.
But here’s what nobody talks about: most parents don’t know what ‘mg/kg’ means. Not because they’re careless-because they’ve never been taught. We hand them a script that says ‘15 mg/kg’ and assume they’ll Google it. They don’t. They guess. They panic. They give too much.
That’s why My Child’s Meds works: it doesn’t make them do math. It makes them do one thing-tap green. Simple. Visual. Human.
And yes, I recommend Pedi STAT to every resident. But I also hand out printed copies of NP Peds MD to every family I see. No app required. No login. Just a laminated card.
Technology is a tool. But the real hero? The parent who calls the pharmacy at midnight because they’re not sure. That’s the behavior we need to encourage-not just the app they use.
And if your app asks for your child’s birthdate to ‘personalize’ the experience? Delete it. That’s not personalization. That’s data mining.
Janice Holmes
January 7, 2026 AT 17:35Okay, but… what if the app glitches? What if the hospital’s system crashes? What if the battery dies during a seizure? What if the app says ‘5 mL’ but the bottle says ‘10 mL’ and you’re half-asleep and your child is screaming and you just want it to STOP?
EVERY SINGLE TIME I’ve used one of these apps, it’s been wrong. Or slow. Or glitchy. Or asked for my child’s zodiac sign.
And don’t get me started on ‘clinically validated’-that’s just a fancy word for ‘we paid a doctor to say it’s okay.’
I once gave my kid 3x the dose because the app said ‘5 mL’ and the syringe had ‘10 mL’ markings and I didn’t realize they were different. The app didn’t warn me. The label didn’t warn me. My panic did.
So now? I keep a laminated card. I write everything by hand. I double-check with my pharmacist. I don’t trust the phone. I trust my eyes. And my hands.
Technology is not the savior. It’s the distraction.
Olivia Goolsby
January 8, 2026 AT 06:21Let’s cut through the noise: this entire ‘pediatric dosing app’ movement is a distraction from the real issue-corporate greed disguised as safety.
Who profits? Apple. Google. The app developers. The hospitals that sell you ‘premium’ versions. The pharmacies that upsell you ‘digital adherence programs.’
Meanwhile, the real problem? The fact that we still use weight-based dosing for children when we know that metabolic differences, genetic polymorphisms, and environmental toxins drastically alter drug clearance. But nope-let’s just tweak the app and call it a day.
And why don’t we have a universal pediatric dosing standard? Because the pharmaceutical industry doesn’t want one. They want you to buy their brand. They want you to trust their app. They want you to think you’re safe… while they profit from every overdose, every ER visit, every lawsuit.
They’re not fixing the system. They’re monetizing your fear.
And if you think My Child’s Meds is ‘free’? Think again. You’re paying with your data. Your child’s health history. Your location. Your sleep patterns. Your panic.
Wake up. This isn’t safety. It’s surveillance.
Alex Lopez
January 9, 2026 AT 02:29Look-I get it. Apps are great. But here’s the thing I learned after my daughter’s hospital stay: the best app is the one you can use when you’re crying, exhausted, and your hands are shaking.
My Child’s Meds? It worked. But the real win? When the nurse printed out a simple table with weight ranges and doses for Tylenol, Motrin, and Benadryl-and taped it to the fridge. No login. No update. No ‘notifications.’ Just a paper chart.
And here’s the kicker: I showed it to my mom, my sister, my babysitter. Everyone could read it. Even the 70-year-old grandma who doesn’t own a smartphone.
So yes, apps are cool. But don’t forget the low-tech solution that’s been saving lives since 1947: a clear, printed, laminated chart.
Also-always, always, always double-check the unit. I once gave a dose based on pounds instead of kg. The app didn’t stop me. My husband did. He saw the syringe and said, ‘That’s not right.’
Technology helps. But human eyes? They’re still the final safety check.
And yes, I still use the app. But I keep the paper. Always.
Gerald Tardif
January 10, 2026 AT 08:06My kid had a seizure last year. We were at home. The ER said ‘give 0.2 mg/kg of diazepam’-but I didn’t know how to calculate it. I called the hospital pharmacy. They walked me through it over the phone. Took 8 minutes. I did it right.
That’s the real tech: someone who cares enough to talk you through it.
Apps? They’re nice. But they’re not magic. I’ve had apps crash mid-dose. I’ve had apps suggest a dose that didn’t match the prescription. I’ve had apps that didn’t recognize my child’s condition.
What saved us? A pharmacist on the line. A printed chart. And me, asking, ‘Are you sure?’
Don’t let the app become your crutch. Let it be your backup. Your safety net. But never your brain.
And if you’re a parent? Learn the formula for epinephrine. Just once. Write it on your bathroom mirror. You might never need it. But if you do? You’ll be glad you did.
Monika Naumann
January 11, 2026 AT 12:34It is profoundly troubling that Western nations export their technological solutions as universal truths, while ignoring the cultural, economic, and epistemological diversity of global caregiving practices. In India, where I am from, we do not rely on apps to administer medicine to our children. We rely on tradition, on intergenerational knowledge, on the wisdom of the family matriarch who has raised five generations.
Our dosing is not based on kilograms, but on the child’s size, appetite, and the rhythm of their breath. We observe. We adjust. We listen.
When we arrived in the U.S., we were told to download apps, to scan barcodes, to input weight, to follow algorithms. We were made to feel inadequate because we did not use them.
But our child thrived.
Perhaps the real problem is not that we lack technology-but that we have forgotten how to trust the human heart.
Let us not confuse efficiency with wisdom. Let us not mistake data for care.
And let us remember: in the quiet of the night, when the child sleeps, no app sings lullabies. Only love does.
Will Neitzer
January 12, 2026 AT 04:52Just read Olivia’s comment and… wow. That’s exactly the fear I had when I first started using the app. I thought, ‘What if the algorithm is wrong?’
But then I remembered: I still have to input the weight. I still have to choose the medication. I still have to confirm the dose before it sends the reminder.
The app doesn’t decide. I do.
It’s like a GPS. It doesn’t drive the car. It just shows you the route. And if you’re not paying attention? You’ll crash.
Same with dosing apps. They’re not magic. They’re mirrors. They reflect your choices.
So yes-double-check the unit. Yes-ask the pharmacist. Yes-keep the paper.
But also… use the app. It’s not the enemy. It’s the ally you didn’t know you needed.