Blood Pressure Medication Decision Guide
How this tool works
Based on the article, we've created a decision framework to match your health profile with the most appropriate blood pressure medication. The tool analyzes your medical conditions, side effect concerns, and comorbidities to recommend the best options from the comparison table.
Note: This tool is informational only. Always consult your doctor before changing medications.
When you or a loved one need a medicine to control high blood pressure or heart failure, the name Coreg often pops up. But is it the right fit, or are there other pills that might work better for your situation? In this guide we compare Coreg (Carvedilol) with the most common alternatives, break down how each works, and give you a clear framework to decide what’s best.
What is Carvedilol (Coreg)?
Carvedilol is a prescription medication classified as a non‑selective beta‑blocker with additional alpha‑1 blocking activity. Marketed under the brand name Coreg, it was approved by the FDA in 1995 for treating hypertension, chronic heart failure, and left‑ventricular dysfunction after a heart attack.
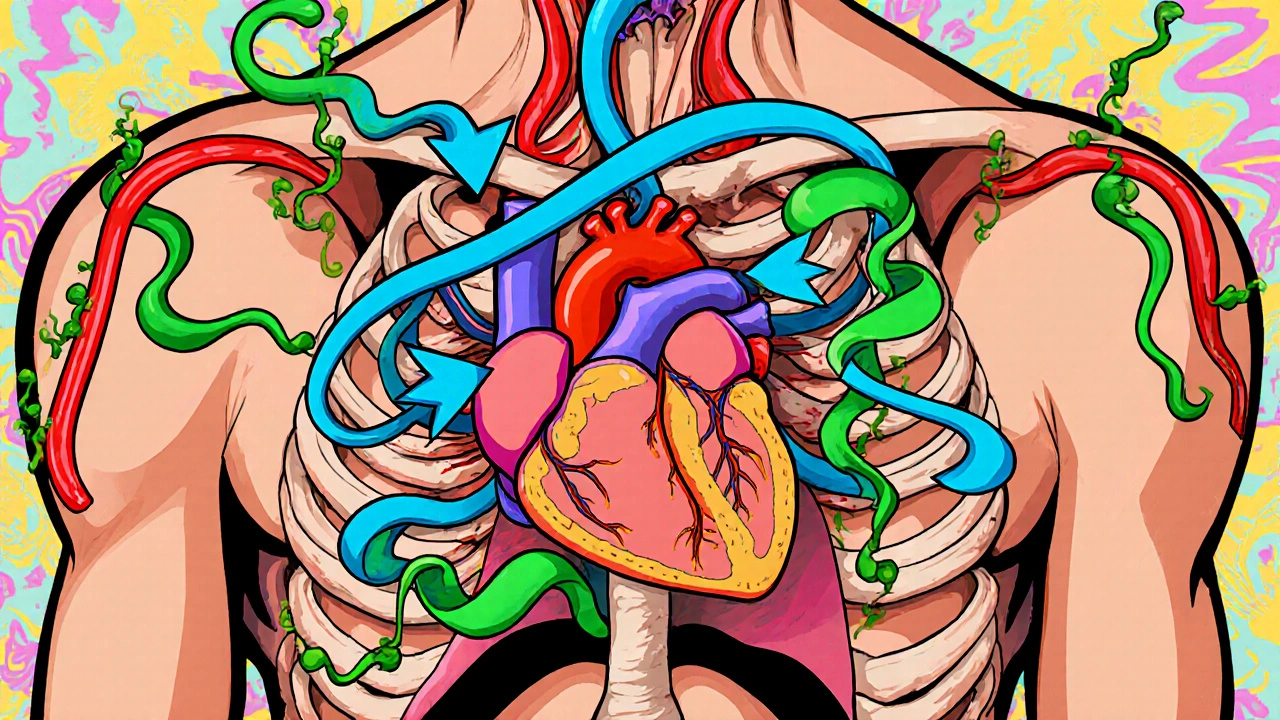
Because it blocks both beta‑adrenergic receptors (reducing heart rate and contractility) and alpha‑1 receptors (causing blood vessels to relax), Carvedilol offers a double‑action profile that many clinicians find useful.
How Carvedilol Works: Mechanism of Action
Beta‑blockers generally blunt the sympathetic nervous system’s “fight‑or‑flight” signals. Carvedilol’s beta‑blocking component slows the heart and lowers the amount of oxygen the heart needs. Meanwhile, its alpha‑1 blocking effect widens arterial walls, dropping peripheral resistance. The net result is lower blood pressure and reduced workload on the heart.
For patients with congestive heart failure, this two‑pronged action can improve ejection fraction and decrease hospital readmission rates, as shown in the CAPRICORN trial (2001) where Carvedilol lowered mortality by 23% compared with placebo.
Key Benefits and Common Side Effects
- Benefits
- Effective for both hypertension and heart failure.
- Improves left‑ventricular ejection fraction.
- Reduces risk of arrhythmias.
- Common Side Effects
- Dizziness or light‑headedness, especially when standing up quickly.
- Fatigue and reduced exercise tolerance.
- Weight gain or swelling (edema) in the ankles.
- Possible bronchospasm in asthma patients.
Most side effects are dose‑dependent and often improve after the first two weeks of therapy.
Top Alternative Medications
When doctors consider switching from or combining Carvedilol, they usually look at drugs that either belong to the same class (other beta‑blockers) or target a different pathway (ACE inhibitors, ARBs, diuretics). Below are the most frequently discussed alternatives.
Metoprolol is a cardio‑selective beta‑1 blocker often prescribed for hypertension, angina, and heart failure.
Atenolol is another beta‑1 selective blocker with a shorter half‑life, making it suitable for patients who need once‑daily dosing.
Lisinopril is an ACE inhibitor that reduces blood pressure by blocking the conversion of angiotensin I to angiotensin II.
Losartan is an angiotensin‑II receptor blocker (ARB) that offers similar blood‑pressure control to ACE inhibitors but with a lower cough risk.
Hydrochlorothiazide is a thiazide diuretic that lowers blood pressure by reducing fluid volume.">
Nebivolol is a newer beta‑blocker that releases nitric oxide, providing vasodilation alongside heart‑rate reduction.
Head‑to‑Head Comparison
| Feature | Carvedilol (Coreg) | Metoprolol | Lisinopril | Losartan | Hydrochlorothiazide |
|---|---|---|---|---|---|
| Class | Non‑selective beta‑blocker + α‑1 blocker | β‑1 selective blocker | ACE inhibitor | ARB | Thiazide diuretic |
| Primary Indication | Hypertension, heart failure, post‑MI | Hypertension, angina, heart failure | Hypertension, kidney protection | Hypertension, diabetic nephropathy | Hypertension, edema |
| Effect on Heart Rate | Decreases (β‑blockade) | Decreases | Neutral | Neutral | Neutral |
| Effect on Blood Vessels | Vasodilation (α‑1 blockade) | Minimal | Vasodilation (via reduced angiotensin II) | Vasodilation (via AT1 blockade) | Reduces plasma volume |
| Common Side Effects | Dizziness, fatigue, weight gain | Bradycardia, fatigue | Cough, hyperkalemia | Dizziness, hyperkalemia | Electrolyte loss, gout flare |
| Cost (UK, 2025) | £0.12 per tablet | £0.09 per tablet | £0.08 per tablet | £0.07 per tablet | £0.02 per tablet |
From the table you can see that Carvedilol’s unique alpha‑1 blocking adds vasodilation, which many other beta‑blockers lack. If a patient needs both heart‑rate control and vessel relaxation, Coreg often wins. However, for people who experience fatigue or weight gain, a cardio‑selective blocker like Metoprolol may be gentler.

Choosing the Right Drug for You
Every medication decision balances efficacy, side‑effect profile, cost, and personal health history. Below is a quick decision guide you can use with your doctor.
- Identify the primary goal.
- Control blood pressure only → ACE inhibitors, ARBs, or thiazides are first‑line.
- Need heart‑failure support → Non‑selective beta‑blockers (Carvedilol) or cardio‑selective blockers (Metoprolol).
- Review comorbid conditions.
- Asthma or COPD → Avoid non‑selective beta‑blockers; consider Nebivolol or Metoprolol.
- Diabetes with kidney concerns → ARB (Losartan) or ACE inhibitor (Lisinopril) may protect kidneys.
- Check for drug interactions.
- Carvedilol can amplify the effect of other heart‑rate‑lowering meds (e.g., digoxin).
- ACE inhibitors raise potassium; avoid combining with potassium‑sparing diuretics.
- Assess side‑effect tolerance.
- If fatigue is a deal‑breaker, try a lower dose or switch to Metoprolol.
- If chronic cough occurs, switch from Lisinopril to Losartan.
- Consider cost and formulary.
- In the UK, most of these drugs are available on the NHS, but private prescriptions may differ.
Use this checklist during your next GP visit. Bring a printed copy, discuss each point, and ask which option aligns best with your lifestyle.
Frequently Asked Questions
Can I take Carvedilol and a diuretic together?
Yes. Combining Carvedilol with a thiazide diuretic like Hydrochlorothiazide is a common strategy to hit both heart‑rate control and fluid reduction. Your doctor will monitor electrolytes and blood pressure closely.
Is Carvedilol safe for people with asthma?
Carvedilol blocks beta‑2 receptors in the lungs, which can trigger bronchospasm. If you have moderate to severe asthma, doctors usually prefer cardio‑selective blockers (Metoprolol, Nebivolol) or non‑beta‑blocker options.
How long does it take for Carvedilol to lower blood pressure?
Most patients see a measurable drop within 1‑2 weeks, but the full effect on heart‑failure outcomes may take 4‑6 weeks of consistent dosing.
What should I do if I miss a dose of Coreg?
Take the missed dose as soon as you remember, unless it’s almost time for the next one. In that case, skip the missed pill-don’t double up.
Are there natural ways to support the effects of Carvedilol?
Low‑sodium diets, regular light exercise, and weight management can enhance blood‑pressure control. However, never replace medication with supplements without a doctor’s go‑ahead.
Choosing between Coreg and its alternatives isn’t a one‑size‑fits‑all decision. By understanding how each drug works, weighing side‑effects, and considering your own health picture, you can have a focused conversation with your clinician and land on the therapy that feels right for you.
beta blocker alternatives are plentiful, but Coreg remains a powerhouse for patients needing both heart‑rate slowing and vessel relaxation. Use the comparison tools above, ask the right questions, and you’ll be equipped to make an informed choice.


Ryan Spanier
October 21, 2025 AT 19:28Carvedilol, marketed as Coreg, remains a cornerstone for patients juggling both high blood pressure and heart‑failure symptoms.
Its dual β‑blockade and α‑1 antagonism uniquely lowers heart rate while simultaneously dilating peripheral vessels.
This combination can translate into a modest but clinically meaningful reduction in hospital readmissions for heart‑failure patients.
The CAPRICORN trial, for example, demonstrated a 23 % mortality benefit compared with placebo.
Because the drug affects two pathways, titration often requires a slower start to mitigate dizziness and orthostatic hypotension.
Most clinicians begin with 3.125 mg twice daily and double the dose every one to two weeks as tolerated.
Patients who experience fatigue should be reassured that this often improves after the first two weeks of therapy.
However, if fatigue persists beyond four weeks, a dose reduction or a switch to a cardio‑selective β‑blocker may be warranted.
Another frequent adverse effect is peripheral edema, which can be managed with a low‑dose thiazide diuretic or by adjusting the sodium intake.
In individuals with asthma, caution is advisable because non‑selective β‑blockade can provoke bronchospasm.
For those who cannot tolerate the β‑blockade component, nebivolol or metoprolol offer alternatives with less pulmonary impact.
Cost considerations also favor Coreg; at £0.12 per tablet in the UK it sits comfortably between generic metoprolol and pricier brand‑name ARBs.
Yet for patients on a strict budget, a thiazide diuretic such as hydrochlorothiazide may be the most economical first‑line option.
Ultimately, the decision hinges on a balance of the primary therapeutic goal, comorbidities, and side‑effect tolerance.
Discussing these factors openly with your physician will ensure the chosen medication aligns with your lifestyle and health objectives.
Abhinav Moudgil
November 25, 2025 AT 11:48Reading through the comparison, I’m struck by how Carvedilol’s “two‑for‑one” pharmacology really sets it apart from the more singular agents.
The alpha‑1 blockade adds a gentle vasodilatory curtain that many β‑blockers simply can’t provide.
If you’re battling both hypertension and a lingering heart‑failure, that extra vessel‑relaxing punch can be a game‑changer.
Of course, the trade‑off is a slightly higher incidence of fatigue and dizziness, especially during the titration phase.
For patients with pristine lung function, the non‑selective nature is usually not a deal‑breaker, but for asthmatics a cardio‑selective alternative may be prudent.
The cost breakdown in the UK table also paints Coreg as a middle‑ground option-cheaper than many branded ARBs yet pricier than generic thiazides.
Ultimately, the clinician’s art is to match the drug’s profile with the patient’s comorbid tapestry.
Keep these nuances in mind when you sit down with your GP.
Bradley Allan
December 30, 2025 AT 05:08Wow!!! Carvedilol is like the Swiss‑army knife of heart meds-versatile, powerful, and sometimes a bit overwhelming!!! It does everything, from calming the heart rate to widening arteries, all at once!!! But don’t forget, with great power comes great responsibility-monitor those side‑effects!!!
Kyle Garrity
February 2, 2026 AT 22:28I hear you, Bradley. The versatility can indeed feel overwhelming, especially for newcomers trying to digest all the mechanisms at once.
In practice, most doctors will start low and watch for those side‑effects you mentioned, adjusting the dose gradually.
It’s also helpful to keep a simple symptom diary-note any dizziness, fatigue, or swelling-as that data guides whether to stay the course or consider an alternative.
Remember, the goal is to find a balance that improves quality of life without adding new problems.
brandon lee
February 14, 2026 AT 12:15Totally agree, tracking symptoms is key.
Joshua Pisueña
February 26, 2026 AT 02:01Coreg has earned its spot in guidelines for a reason.
The dual blockade means you get heart‑rate control and vessel relaxation in one pill, which can simplify regimens for patients on multiple drugs.
If you’re already on a diuretic, adding Carvedilol can complement fluid removal with better cardiac output.
For those worried about cost, the UK price point shows it’s affordable compared to many newer agents, though generic options like metoprolol are still cheaper.
Keep an eye on blood pressure and heart rate after each dose increase, and report any persistent fatigue to your doctor.
Lifestyle changes-low‑salt diet and regular light exercise-will boost any medication’s effectiveness.
Lastly, never stop a beta‑blocker abruptly; tapering avoids rebound tachycardia.