Clopidogrel-PPI Interaction Checker
Select Your Situation
This tool will help you determine the safest proton pump inhibitor to take while on clopidogrel based on your bleeding risk factors.
Your PPI Recommendations
PPIs reduce bleeding risk by 69% in high-risk patients on dual antiplatelet therapy
Recommended PPIs
Minimal interaction with clopidogrel
Minimal interaction with clopidogrel
Unrecommended PPIs
Severely reduces clopidogrel effectiveness
Severely reduces clopidogrel effectiveness
When you take clopidogrel after a heart attack or stent placement, your blood is thinner-on purpose. It stops clots from forming inside your arteries. But if you’re also taking a proton pump inhibitor (PPI) for heartburn or stomach ulcers, that thinning effect might not work as well. And not all PPIs are created equal. Some can seriously weaken clopidogrel’s power. Others? They barely touch it.
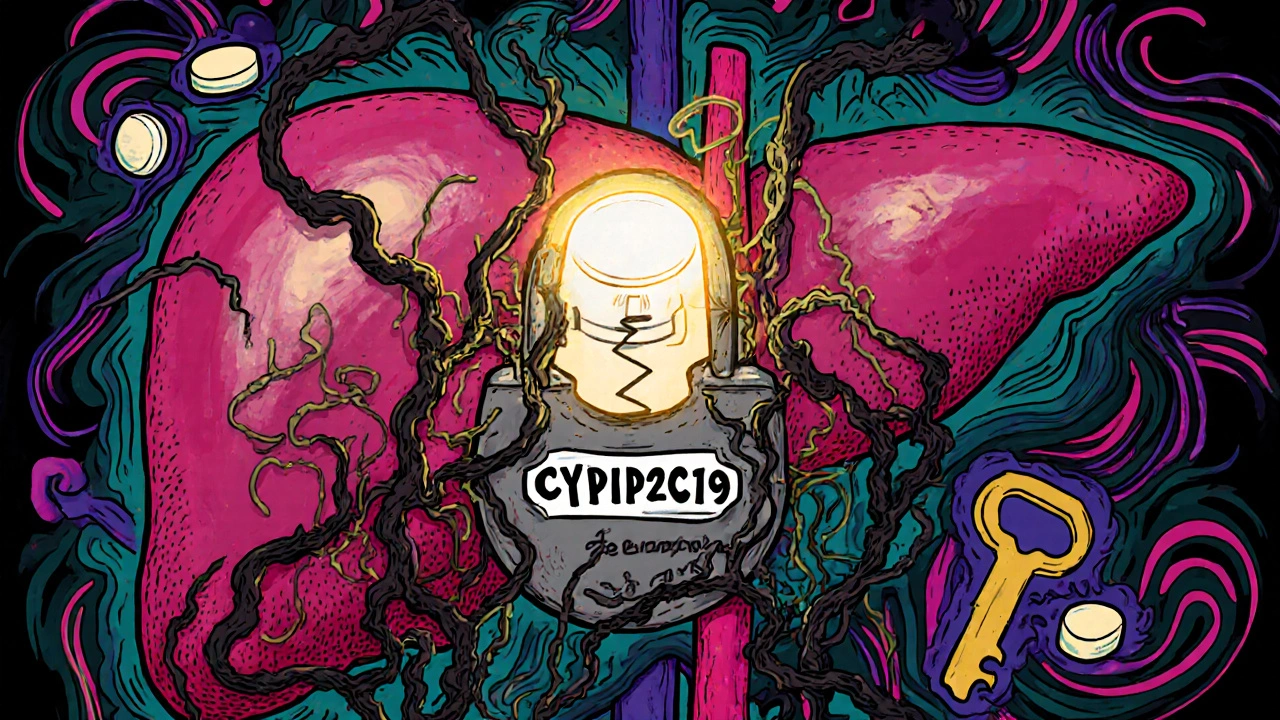
Why Clopidogrel Needs Help to Work
Clopidogrel isn’t active when you swallow it. Your liver has to turn it into its real form-the one that blocks platelets from sticking together. That job falls to an enzyme called CYP2C19. If that enzyme is blocked, clopidogrel stays useless. And that’s exactly what happens with certain PPIs.Think of it like a key (clopidogrel) that needs a special lock (CYP2C19) to unlock its effect. Some PPIs jam that lock. Omeprazole and esomeprazole are the worst offenders. They bind tightly to CYP2C19, leaving little room for clopidogrel to get processed. Studies show omeprazole can cut clopidogrel’s active metabolite by nearly half. In one study, platelet inhibition dropped from 84% to 51% when patients took both drugs. One patient in that trial had no antiplatelet effect at all-even when the drugs were taken 12 hours apart.
Not All PPIs Are the Same
This isn’t a blanket problem. It’s specific to certain drugs. Omeprazole and esomeprazole are the big red flags. But pantoprazole, rabeprazole, and lansoprazole? They barely interfere.Here’s why: their chemical structure doesn’t grip CYP2C19 the same way. Rabeprazole has a half-life of just 1-2 hours. It comes and goes fast, giving CYP2C19 room to do its job. Pantoprazole? It’s weak at blocking the enzyme. Studies show it doesn’t reduce clopidogrel’s effectiveness. In fact, platelet inhibition stayed in the safe, therapeutic range (35-45%) with rabeprazole, while omeprazole pushed it below 20%-dangerously low.
Real-world data backs this up. A 2020 analysis found that when doctors switched patients from omeprazole to pantoprazole, inappropriate prescribing dropped from 21% to under 9%. That’s not coincidence. It’s clinical adaptation.
What the Guidelines Say (And Why They’re Mixed)
You’ll find conflicting advice if you look around. The FDA warned in 2009: avoid omeprazole with clopidogrel. The European Medicines Agency followed. But then came the COGENT trial in 2010. It showed no increase in heart attacks or death when omeprazole was added to clopidogrel-even though lab tests showed reduced platelet inhibition.That’s the heart of the confusion. Lab results say one thing. Real patients say another. Dr. Deepak Bhatt’s research found a 50% higher risk of heart attacks or death with PPI use. But Dr. Dominick Angiolillo and others argue that CYP2C19 gene variations matter more than PPIs-and those variations don’t reliably predict outcomes.
The American College of Cardiology and the European Society of Cardiology now agree on one thing: avoid omeprazole and esomeprazole. But they say pantoprazole and rabeprazole are safe. The NHS Specialist Pharmacy Service says it plainly: "Other PPIs are considered safe with clopidogrel."

Who Needs a PPI Anyway?
You don’t take a PPI just because you can. You take it because you’re at high risk for bleeding. The numbers tell you who’s most vulnerable:- Age 75 or older: 3 times more likely to bleed
- History of stomach ulcer: 13 times more likely
- Taking NSAIDs like ibuprofen: 4 times more likely
- H. pylori infection: doubles your risk
For these people, skipping the PPI is riskier than the interaction. A 2017 study showed PPIs cut GI bleeding risk by 69% in patients on dual antiplatelet therapy. That’s huge. If you’re 78, on aspirin and clopidogrel, and have a history of ulcers, not taking a PPI could kill you faster than the drug interaction ever could.
What Should You Do?
If you’re on clopidogrel and need a PPI, here’s what works:- Don’t take omeprazole or esomeprazole. Ever.
- Choose pantoprazole or rabeprazole. They’re the safest bets.
- Lansoprazole is okay if the others aren’t available, but it’s not ideal.
- Don’t try to space out doses. Taking clopidogrel in the morning and omeprazole at night doesn’t fix the problem. The enzyme stays blocked.
- Ask your pharmacist or doctor to check your meds. Many people don’t realize their heartburn pill is weakening their heart drug.
And if you’re not sure whether you even need a PPI? Ask. Many people take them long-term without a clear reason. A 2023 review found nearly 40% of PPI prescriptions are inappropriate. If your stomach feels fine and you’re not on NSAIDs or steroids, you might be able to stop it.

What’s Next? New Drugs Are Coming
The tide is turning. New antiplatelet drugs like ticagrelor and prasugrel don’t rely on CYP2C19. They work directly. That’s why the 2023 European guidelines now recommend ticagrelor over clopidogrel for most heart attack patients. If you’re starting therapy now, your doctor might skip clopidogrel entirely.And if you need acid control? There’s vonoprazan-a new type of acid blocker that doesn’t touch CYP2C19. It’s in phase III trials and could be available soon. It’s stronger than PPIs, works faster, and won’t interfere with your heart meds.
Bottom Line: Don’t Panic, But Don’t Ignore It
The science isn’t perfect. Some studies say the interaction matters. Others say it doesn’t. But we know this: omeprazole and esomeprazole block clopidogrel’s activation in the lab. We know patients on those combinations have higher platelet activity. We know that in high-risk people, skipping PPIs leads to more bleeding. We know pantoprazole and rabeprazole don’t cause the same problem.So don’t stop your meds. Don’t assume your doctor knows this. Ask: "Is my heartburn medicine weakening my heart drug?" If they say yes to omeprazole, ask for a switch. Your life might depend on it.
Does omeprazole really make clopidogrel less effective?
Yes. Omeprazole strongly inhibits the CYP2C19 enzyme your liver needs to activate clopidogrel. Studies show it can reduce the drug’s active metabolite by up to 47%, leading to significantly higher platelet activity. This effect happens even if the drugs are taken 12 hours apart.
Can I take pantoprazole with clopidogrel?
Yes. Pantoprazole has minimal effect on CYP2C19 and does not reduce clopidogrel’s antiplatelet action. It’s the preferred PPI when you need acid control while on clopidogrel. Multiple studies and guidelines, including those from the NHS and ESC, confirm it’s safe.
What if I’ve been taking omeprazole with clopidogrel for years?
Talk to your doctor before stopping or switching. If you’re at low risk for GI bleeding, you might not need a PPI at all. If you’re high risk (e.g., over 75, history of ulcers, on NSAIDs), switch to pantoprazole or rabeprazole. Don’t stop clopidogrel-your risk of clotting is far greater than the risk of switching PPIs.
Are there alternatives to clopidogrel that don’t interact with PPIs?
Yes. Ticagrelor and prasugrel are newer antiplatelet drugs that don’t rely on CYP2C19 for activation. They work directly and aren’t affected by PPIs. The 2023 European guidelines now recommend ticagrelor over clopidogrel for most patients with acute coronary syndrome.
Should I get tested for CYP2C19 gene variants?
Not routinely. While poor metabolizers of CYP2C19 do respond worse to clopidogrel, studies haven’t shown that testing improves outcomes enough to justify the cost. The bigger issue is avoiding omeprazole and esomeprazole. If you’re on those, switching PPIs matters more than genetic testing.

Jeremy Samuel
November 20, 2025 AT 20:19Nicole Ziegler
November 22, 2025 AT 06:53Destiny Annamaria
November 24, 2025 AT 05:58Alyssa Torres
November 24, 2025 AT 07:38Kristi Bennardo
November 25, 2025 AT 15:46Matthew Karrs
November 26, 2025 AT 22:49Aruna Urban Planner
November 27, 2025 AT 03:14Bharat Alasandi
November 27, 2025 AT 07:49Ravi boy
November 27, 2025 AT 23:58Dana Oralkhan
November 29, 2025 AT 18:41Gerald Cheruiyot
November 30, 2025 AT 21:16Michael Fessler
December 1, 2025 AT 08:52Summer Joy
December 2, 2025 AT 04:11Liam Strachan
December 2, 2025 AT 23:02Ron and Gill Day
December 4, 2025 AT 22:31