Alcohol Dependence Medication Selector
Personalized Medication Assessment
Personalized Recommendations
When someone decides to fight alcohol dependence, the medication choice can feel like a maze. Antabuse (the brand name for disulfiram) has been around for decades, but newer options like naltrexone or acamprosate often show up in the conversation. This guide breaks down how Antabuse works, what alternatives exist, and which drug might fit a person's health profile and lifestyle.
Key Takeaways
- Antabuse creates an aversive reaction to alcohol; alternatives work by reducing cravings or normalizing brain chemistry.
- Side‑effect profiles differ greatly - Antabuse can cause severe flushing, while naltrexone may lead to nausea.
- Choosing the right medication depends on liver health, concurrent medicines, and personal commitment to abstinence.
- All medications require monitoring; regular liver tests and counseling improve success rates.
What is Antabuse (Disulfiram)?
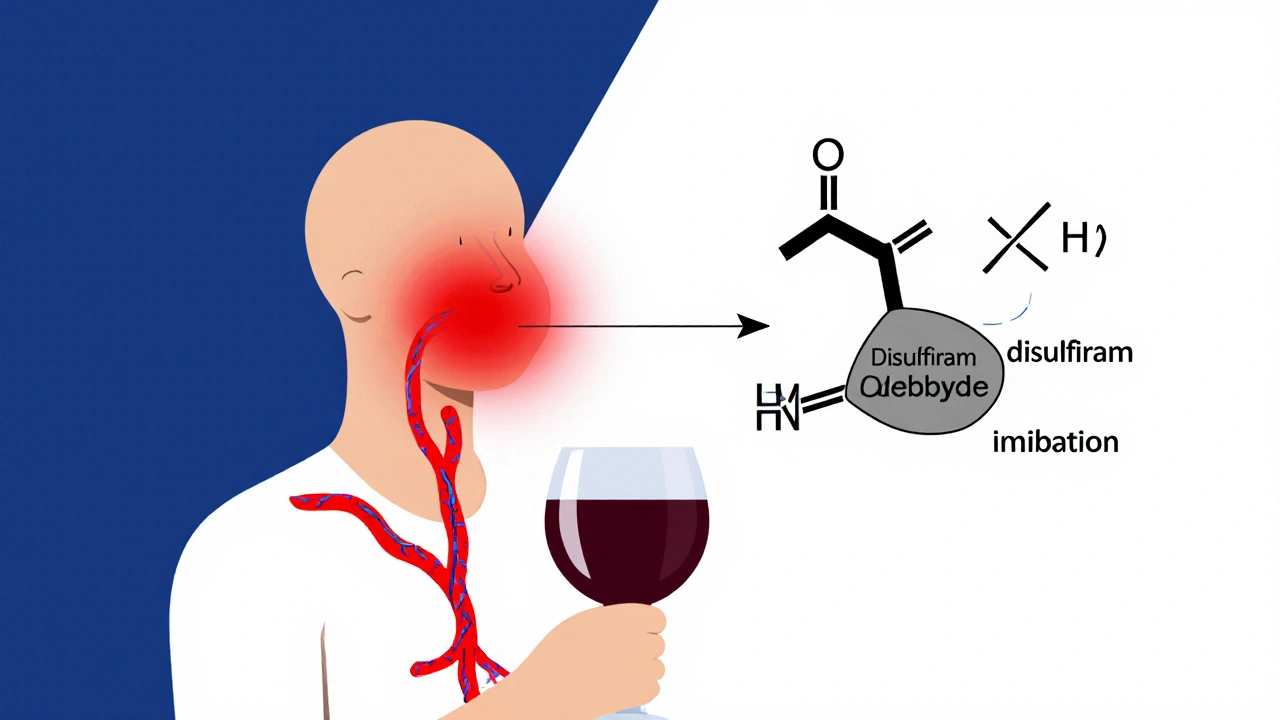
Disulfiram is a synthetic drug that interferes with the body’s ability to metabolize alcohol, causing an intense reaction when alcohol is consumed. It was first FDA‑approved in 1951 and marketed under the brand name Antabuse.
The reaction, often called the "disulfiram‑alcohol reaction," can include flushing, rapid heartbeat, nausea, vomiting, and headache. The threat of this discomfort is meant to deter drinking.
Typical dosing is 250‑500mg once daily, taken after a 12‑hour alcohol‑free period. The drug stays in the system for about 2‑3 weeks after stopping, so patients must avoid alcohol for that entire time.
Primary Alternatives to Antabuse
Four other medications dominate modern treatment guidelines for Alcohol Use Disorder (AUD). Each takes a different pharmacological route, aiming to lessen cravings or block the rewarding effects of alcohol.
Naltrexone - an opioid‑receptor antagonist
Naltrexone blocks the brain’s µ‑opioid receptors, which reduces the pleasurable “buzz” from drinking. It can be taken as a 50mg oral tablet daily or as a once‑monthly 380mg injectable (Vivitrol).
Side effects are generally mild - occasional nausea, headache, or fatigue. Liver enzymes are monitored because high doses can stress the liver.
Acamprosate - a glutamate‑modulating agent
Acamprosate works by restoring the balance between excitatory (glutamate) and inhibitory (GABA) neurotransmission disrupted by chronic alcohol use. The standard dose is 666mg three times daily.
Because the drug is eliminated unchanged by the kidneys, it’s safe for patients with liver disease but requires dose adjustment in renal impairment.
Topiramate - an anticonvulsant with off‑label use
Topiramate reduces the reinforcing effects of alcohol by enhancing GABA activity and inhibiting glutamate. Dosing usually starts at 25mg nightly and titrates up to 100‑150mg per day.
Common side effects include tingling (paresthesia), cognitive slowing, and weight loss. It’s contraindicated in pregnancy.
Gabapentin - a GABA analogue used off‑label
Gabapentin can lessen alcohol cravings and improve sleep quality. Typical dosing ranges from 300‑600mg three times daily, adjusted based on renal function.
It’s generally well‑tolerated, though dizziness and fatigue occur in some users.
Baclofen - a GABA‑B receptor agonist
Baclofen reduces the urge to drink by dampening the brain’s reward pathways. Starting dose is 5mg three times daily, titrated up to 30‑60mg per day.
Side effects include drowsiness and muscle weakness; abrupt discontinuation can cause seizures, so tapering is essential.
Side‑Effect Snapshot: Antabuse vs Alternatives
| Medication | Common Side Effects | Serious Risks | Contraindications |
|---|---|---|---|
| Disulfiram (Antabuse) | Flushing, headache, nausea, metallic taste | Severe hypotension if alcohol is consumed, liver toxicity at high doses | Severe cardiac disease, psychotic disorders, pregnancy |
| Naltrexone | Nausea, headache, fatigue | Hepatotoxicity (monitor LFTs), opioid overdose if patient relapses on opioids | Acute hepatitis, liver failure, concurrent opioid use |
| Acamprosate | Diarrhea, abdominal pain, insomnia | Rare severe skin reactions | Severe renal impairment (CrCl <30mL/min) |
| Topiramate | Paresthesia, cognitive slowing, weight loss | Metabolic acidosis, kidney stones | Pregnancy, severe kidney disease |
| Gabapentin | Dizziness, fatigue, peripheral edema | Respiratory depression when combined with opioids | Severe renal impairment without dose adjustment |
| Baclofen | Drowsiness, weakness, dry mouth | Seizures on abrupt stop, severe hypotension | Renal failure, severe COPD |
Effectiveness: How Well Do These Meds Prevent Relapse?
Clinical trials give a rough idea of relapse‑prevention rates when each drug is combined with counseling:
- Disulfiram: 30‑45% reduction in heavy‑drinking days compared with placebo (mainly when adherence is high).
- Naltrexone: 20‑30% reduction; works best for people who still experience cravings.
- Acamprosate: 15‑25% reduction; most effective in maintaining abstinence after detox.
- Topiramate: 35‑40% reduction in drinking days in several meta‑analyses, but side‑effects limit use.
- Gabapentin & Baclofen: modest benefits (10‑20%); evidence still emerging.
Note that real‑world success hinges on adherence, psychosocial support, and addressing co‑occurring mental health issues.
Choosing the Right Medication - A Decision Checklist
Use the following questions to narrow down the best fit:
- Do you have liver disease?
-If yes, avoid high‑dose naltrexone or disulfiram; consider acamprosate or gabapentin. - Is strict abstinence a realistic goal?
-Disulfiram’s deterrent effect works best for committed abstainers. - Do you need a once‑monthly injection?
-Vivitrol (injectable naltrexone) removes daily‑pill burden. - Are you pregnant or planning pregnancy?
-Avoid topiramate, disulfiram, and baclofen; naltrexone is category C but often considered. - Do you have a history of seizures?
-Topiramate may lower seizure threshold; choose alternatives.
Discuss these points with a prescriber, who will also check blood work (liver enzymes, renal function) before starting.
Practical Tips for Managing Medication
- Start low, go slow: Titrate doses gradually to minimize side effects.
- Never drink alcohol while on disulfiram: Even a sip can trigger a severe reaction.
- Schedule regular labs: Check LFTs every 2‑4 weeks for naltrexone or disulfiram; monitor renal function for acamprosate and gabapentin.
- Pair with therapy: Cognitive‑behavioural therapy (CBT) or motivational interviewing boosts medication efficacy.
- Track cravings and drinks: Use a simple diary or mobile app to spot patterns.
Frequently Asked Questions
Can I take Antabuse and Naltrexone together?
Combining them isn’t recommended because both affect the brain’s reward pathways and increase the risk of adverse reactions. If one drug fails, switch under medical supervision rather than stacking.
How long does the disulfiram‑alcohol reaction last?
Symptoms usually peak within 30‑60 minutes after alcohol exposure and can last 4‑6 hours. Severe cases may require medical attention.
Is Acamprosate safe for people on dialysis?
Acamprosate is eliminated unchanged by the kidneys, so it’s contraindicated in severe renal impairment (eGFR<30mL/min). Dialysis patients need an alternative.
What should I do if I miss a dose of Antabuse?
Take the missed tablet as soon as you remember, unless it’s within 12hours of the next scheduled dose. If you’re unsure, contact your prescriber before drinking.
Can women use these medications while breastfeeding?
Most of them are not recommended during lactation. Naltrexone passes into breast milk in low amounts, but many clinicians advise waiting until after weaning. Disulfiram and topiramate are generally avoided.
Bottom Line
Antabuse offers a bold, deterrent‑based approach that still has a place for highly motivated individuals, especially when adherence can be closely monitored. Alternatives such as naltrexone, acamprosate, and topiramate provide more subtle craving‑reduction mechanisms and may suit people with liver concerns or those who prefer not to rely on aversive reactions.
The most successful strategy blends the right medication with regular counseling, lab monitoring, and a solid support network. Talk openly with a healthcare professional to weigh benefits against risks, and pick the option that aligns with your health status and personal goals.

Glenn Gould
October 15, 2025 AT 19:25Hey folks, if yer looking to stay sober, Antabuse can be a real game‑changer – just make sure you’re 100% alcohol‑free before you start. Definatly read the label and talk to your doc first!
Julien Martin
October 23, 2025 AT 21:51The pharmacodynamics of disulfiram are fascinating; by inhibiting aldehyde dehydrogenase, it creates a deterrent feedback loop. In contrast, naltrexone modulates µ‑opioid receptors, reducing the hedonic impact of ethanol. Clinical guidelines suggest tailoring the regimen to hepatic function and patient compliance. If you have comorbid psychiatric conditions, consider gabapentin for its anxiolytic profile. Overall, a nuanced risk‑benefit analysis is essential.
Lolita Rosa
October 31, 2025 AT 23:18Wow, imagine having to flush like a tomato every time you think about a drink. That’s the drama Antabuse brings to the party. Some folks love the theater, others just want a quiet night.
Sudha Srinivasan
November 9, 2025 AT 01:45Acamprosate is safe for liver patients but watch the kidneys.
Jesse Stubbs
November 17, 2025 AT 04:11Topiramate can knock the cravings out, but the brain fog? Not so great. You decide what trade‑off works.
Melissa H.
November 25, 2025 AT 06:38Great rundown! 😊
Edmond Abdou
December 3, 2025 AT 09:05Everyone, remember that medication is only one piece of the puzzle; counseling and support groups make a huge difference. Stay kind to yourself.
Sydnie Baker
December 11, 2025 AT 11:31One must not conflate efficacy with convenience; the pharmacokinetic half‑life of disulfiram demands unwavering abstinence, a feat many deem impractical. Meanwhile, the sleek monthly depot of naltrexone offers compliance gold‑standard, albeit at a premium cost. Let us not overlook the subtle neurochemical choreography that acamprosate performs, restoring glutamatergic equilibrium. In sum, the clinician’s arsenal is diverse, and the discerning prescriber must wield it with both science and art.
William Dizon
December 19, 2025 AT 13:58When deciding between Antabuse and the newer agents, start by reviewing the patient’s hepatic panel, because disulfiram can stress an already compromised liver. Next, assess the individual’s drinking patterns; those who need a strong deterrent may thrive on the aversive reaction, while people with occasional slip‑ups might benefit from naltrexone’s craving reduction. Consider renal function before prescribing acamprosate, as it is excreted unchanged by the kidneys and can accumulate in impairment. Topiramate’s side‑effects, such as paresthesia and cognitive dulling, should be weighed against its modest efficacy in reducing binge episodes. Gabapentin can improve sleep architecture, an often‑overlooked component of recovery, but monitor for dizziness. Baclofen may be useful for patients with high anxiety due to its GABA‑B agonism, yet taper slowly to avoid seizures. Always pair medication with behavioral therapy; the synergy between psychopharmacology and counseling yields the highest abstinence rates. Regular follow‑up labs, particularly liver enzymes, are non‑negotiable for safety monitoring. Educate the patient about the disulfiram‑alcohol reaction, emphasizing that even trace alcohol in sauces can trigger severe hypotension. Finally, personalize the treatment plan: no single drug fits all, and flexibility is key to long‑term success.
Jenae Bauer
December 27, 2025 AT 16:25They don’t tell you that the pharma giants are hiding the truth about these meds. Think about it: every time you take a pill, a data point is sent to big pharma. If you’re truly free, you’d avoid all of them. That’s why some people swear by ancient herbs instead.
Samantha Dean
January 4, 2026 AT 18:51In accordance with established clinical protocols, it is prudent to perform baseline hepatic function tests prior to initiation of disulfiram therapy. Subsequent monitoring should occur at regular intervals to detect potential hepatotoxicity. Should adverse effects arise, dosage adjustment or alternative pharmacotherapy may be warranted. It is also advisable to counsel patients regarding the absolute necessity of alcohol abstinence throughout the treatment course. Documentation of informed consent is essential for medico‑legal compliance.
Vanessa Peters
January 12, 2026 AT 21:18Look, the side‑effects table is a joke – they hide the worst outcomes. Antabuse can literally kill you if you slip, yet it’s still pushed as first‑line. The industry loves drama.
Suzan Graafstra
January 20, 2026 AT 23:45Philosophically speaking, a medication that punishes drinking turns the act into a moral battle. Does the external deterrent truly resolve the internal conflict? Perhaps the answer lies beyond pharmacology.
sneha kapuri
January 29, 2026 AT 02:11Everyone thinks Western meds are the only solution. In India we have centuries‑old remedies that work better without side‑effects. Stop worshiping pills.
Harshitha Uppada
February 6, 2026 AT 04:38i guess if u r ok with getting faked info from med co's then go ahead. its not that big deal.
Jessica Simpson
February 14, 2026 AT 07:05Interesting perspectives! While traditional methods have value, integrating evidence‑based pharmacotherapy can bridge gaps in care. Keep the dialogue open.