When you need a medication for bone conditions, the market can feel like a maze. Didronel (Etidronate) is a bisphosphonate that’s been used for decades to slow down bone turnover. But is it the right choice for you, or should you look at newer options? This guide walks through how Didronel works, what the main alternatives are, and which factors matter most when you compare them.
What is Didronel (Etidronate) and how does it work?
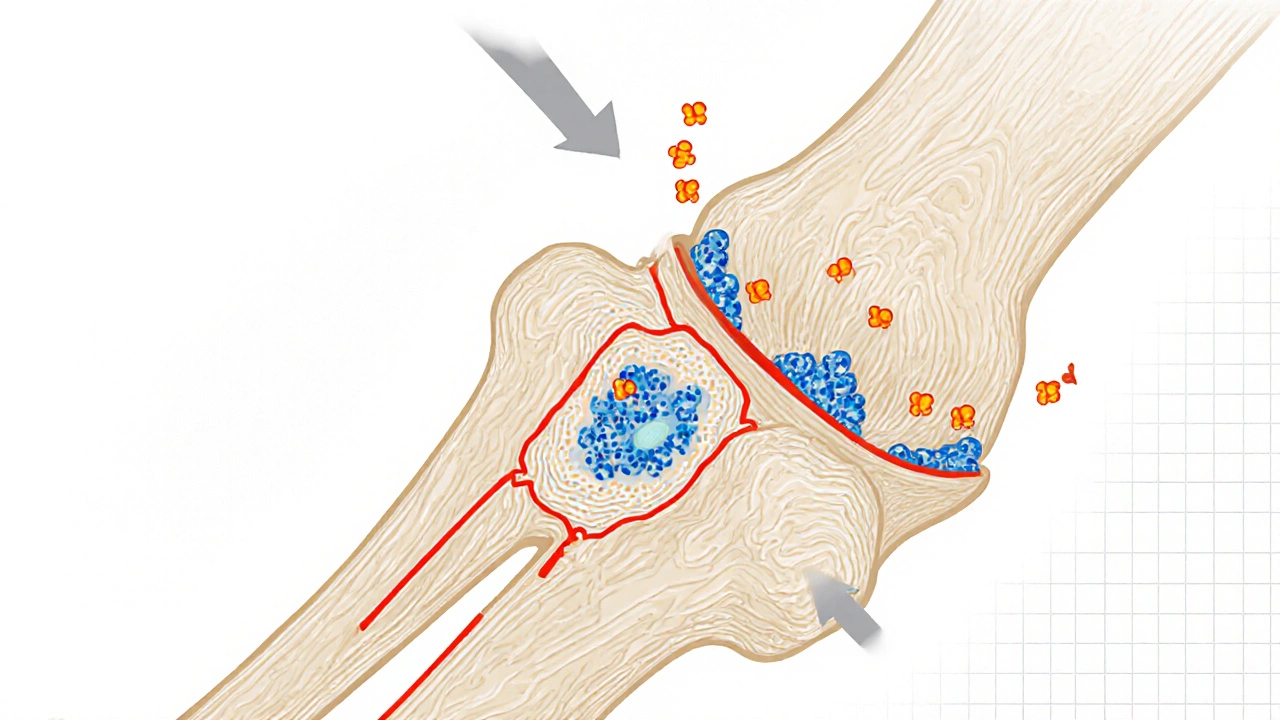
Didronel (Etidronate) belongs to the first‑generation bisphosphonate class. It binds to hydroxyapatite crystals in bone and blocks the activity of osteoclasts - the cells that break down bone tissue. By limiting resorption, it helps maintain bone mineral density (BMD) over time.
Typical UK dosing for Paget’s disease is 400mg twice daily for two weeks, followed by a maintenance dose of 400mg once daily for another two weeks. For preventing kidney stones in hypercalcemia, the dose is often lower - 400mg twice daily for two weeks only.
Why compare? The main reasons to look at alternatives
Even though Didronel is inexpensive and widely available on the NHS, it has a few downsides that push patients and doctors toward newer agents. The most common reasons are:
- Better potency - newer bisphosphonates reduce fracture risk more dramatically.
- More convenient dosing - weekly or monthly tablets versus two‑week courses.
- Fewer gastrointestinal (GI) side effects - some patients can’t tolerate the acidic tablet.
- Specific approvals - certain drugs are licensed for osteoporosis, others for metastatic bone disease.
Below we cover the five most frequently mentioned alternatives in the UK: alendronate, risedronate, pamidronate, zoledronic acid, and denosumab.
Quick look at the alternatives
- Alendronate - a second‑generation oral bisphosphonate taken weekly.
- Risedronate - similar to alendronate but can be taken daily, weekly, or monthly.
- Pamidronate - an intravenous bisphosphonate usually given every 3‑4 weeks for cancer‑related bone disease.
- Zoledronic acid - a potent IV drug given once a year for osteoporosis or every 3‑4 weeks for malignancy.
- Denosumab - a monoclonal antibody injected subcutaneously every 6 months, approved for both osteoporosis and bone metastases.
Side‑by‑side comparison table
| Drug | Generation / Class | Typical Indication (UK) | Route & Dosing Frequency | Potency (fracture reduction) | Approx. NHS Cost (per year) | Key Side Effects |
|---|---|---|---|---|---|---|
| Didronel (Etidronate) | 1st‑gen bisphosphonate | Paget’s disease, hypercalcaemia | Oral - 2‑week course, then 2‑week maintenance | Low - modest BMD gain | ~£30 | GI upset, rare osteomalacia with long‑term use |
| Alendronate | 2nd‑gen bisphosphonate | Post‑menopausal osteoporosis | Oral - 70mg weekly | High - ~45% fracture risk reduction | ~£60 | Esophageal irritation, atypical femur fracture (rare) |
| Risedronate | 2nd‑gen bisphosphonate | Osteoporosis, glucocorticoid‑induced bone loss | Oral - 35mg weekly or monthly | High - comparable to alendronate | ~£65 | GI upset, renal function monitoring needed |
| Pamidronate | IV bisphosphonate | Bone metastases, hypercalcaemia of malignancy | IV - 90mg every 3‑4weeks | Very high for malignant bone pain | ~£250 | Flu‑like symptoms, transient hypocalcaemia |
| Zoledronic acid | IV bisphosphonate (potent) | Osteoporosis (annual) & cancer‑related bone disease (q3‑4weeks) | IV - 5mg once yearly (osteoporosis) or 4mg q3‑4weeks (cancer) | Very high - 50‑70% fracture reduction | ~£200 (annual dose) | Acute phase reaction, renal toxicity at high doses |
| Denosumab | RANKL inhibitor (monoclonal antibody) | Osteoporosis, bone metastases, giant cell tumour | SC - 60mg every 6months | High - similar to zoledronic acid | ~£350 (annual) | Skin reactions, rare osteonecrosis of jaw |

When Didronel might still be the right pick
If you’re being treated for Paget’s disease, Didronel remains the first‑line NHS option because it’s cheap and the dosing schedule fits the disease’s intermittent nature. It’s also the only bisphosphonate approved for preventing certain types of kidney stones caused by high calcium levels.
For patients with severe renal impairment (eGFR <30mL/min), oral Didronel is sometimes tolerated better than many newer bisphosphonates, which require stricter renal monitoring.
Why the newer drugs often win for osteoporosis
Osteoporosis guidelines (e.g., NICE NG56) now recommend a weekly or monthly oral bisphosphonate or an annual IV infusion for most post‑menopausal women. The evidence shows a larger reduction in vertebral and hip fractures compared with Didronel’s modest BMD gains.
Convenience matters, too. A once‑yearly infusion of zoledronic acid means you hardly have to think about medication adherence, which is a big win for busy patients.
Practical factors to weigh before you decide
- Cost & reimbursement: Didronel is cheap, but the NHS may fund a more effective drug if you meet fracture‑risk criteria.
- Dosing convenience: If you hate swallowing pills, an IV or SC option could be easier.
- Side‑effect profile: GI irritation is common with oral bisphosphonates; IV drugs may cause flu‑like reactions.
- Renal function: Check eGFR; some IV bisphosphonates are contraindicated if kidney function is low.
- Future pregnancy: Women planning pregnancy should avoid most bisphosphonates; discuss timing with your GP.
Always bring a recent bone density scan (DXA) and blood tests (calcium, renal panel) to the appointment - they help the clinician match the right drug to your risk profile.
How to talk to your doctor about switching
- Ask about your current fracture risk score (FRAX). If it’s high, a more potent drug may be justified.
- Bring up any GI problems you’ve had with tablets - that can tip the balance toward an IV or SC option.
- Clarify how often you’re willing to attend a clinic. Once‑yearly infusions are great if you dislike frequent visits.
- Discuss cost concerns openly. The NHS will usually cover the most effective choice for your condition, but private patients need to know the price difference.
Key take‑aways
- Didronel (Etidronate) is inexpensive and works well for Paget’s disease and hypercalcaemia.
- For osteoporosis, newer bisphosphonates (alendronate, risedronate) or IV agents (zoledronic acid, denosumab) provide stronger fracture protection.
- Side‑effect and dosing preferences often decide the winner - consider GI tolerance, renal function, and how often you want to take medication.
- Always have a recent DXA scan and blood work handy when discussing options with your GP or specialist.
Frequently Asked Questions
Can I take Didronel and alendronate together?
No. Both are bisphosphonates and work on the same pathway. Combining them offers no extra benefit and raises the risk of side effects such as esophageal irritation and jaw osteonecrosis.
Is Didronel safe for people with kidney disease?
Didronel is less likely to accumulate in the kidneys than newer IV bisphosphonates, so it can be an option for mild to moderate renal impairment. However, dosing should be adjusted and kidney function monitored regularly.
How long does it take for Didronel to show effect on bone density?
Significant changes in BMD usually appear after 6‑12months of continuous therapy, but the biggest benefit for Paget’s disease is reduced bone turnover, which can be seen in blood markers within a few weeks.
Why do some patients prefer a yearly infusion of zoledronic acid?
The once‑yearly schedule eliminates the need for daily or weekly pills, which improves adherence. It also provides a stronger reduction in hip and vertebral fractures compared with many oral options.
Is denosumab a good alternative if I cannot tolerate oral bisphosphonates?
Yes. Denosumab is given as a subcutaneous injection every six months and bypasses the GI tract entirely. It’s an effective choice for osteoporosis, but you’ll need regular monitoring for calcium levels and dental health.

Johnpaul Chukwuebuka
October 16, 2025 AT 18:17Didronel is cheap but kinda harsh on the tummy.
Xavier Hernandez
October 18, 2025 AT 01:00When you pick a bone‑health drug, you’re not just saving a few pennies; you’re playing with the very scaffolding of your skeleton. The cheapness of Didronel might lull some into thinking it’s a free ride, but the GI irritation and modest potency betray that illusion. Newer bisphosphonates like alendronate and risedronate hug the bone tighter and spare the stomach more mercifully. If you’re looking for a drug that respects both your wallet and your wellbeing, aim higher than a two‑week course of etidronate. Remember, convenience and safety should never be sacrificed at the altar of cost.
ANTHONY COOK
October 19, 2025 AT 07:41Listen up, folks – Didronel’s ancient dosing schedule is a relic from the stone age 😒. You gulp pills every other day for two weeks and then hope the bones magically cooperate. The GI fallout alone can turn a simple breakfast into a battlefield. Modern alternatives give you a weekly pill or an injection and keep the stomach drama down to zero.
Sarah Aderholdt
October 20, 2025 AT 14:23If you’re managing Paget’s, Didronel still tops the NHS list because it hits the disease’s intermittent flare‑ups. For anything else, the newer agents pull ahead on potency.
Phoebe Chico
October 21, 2025 AT 21:05Hey bone‑enthusiasts, Didronel might be the budget hero, but it’s like borrowing a flip‑phone in a smartphone world. You get the job done for stone‑prevention, yet you’ll miss out on the sleek, once‑a‑year zap that zoledronic acid offers. Keep eyes open for what fits your lifestyle!
Larry Douglas
October 23, 2025 AT 03:46The pharmacokinetic profile of etidronate demonstrates a relatively low affinity for hydroxyapatite when compared with second‑generation bisphosphonates; consequently, its anti‑resorptive effect remains modest. Moreover, the required two‑week cycling regimen poses adherence challenges, especially in patients with comorbid gastrointestinal sensitivities. Clinical guidelines therefore preferentially recommend alendronate or risedronate for primary osteoporosis prevention, reserving Didronate for specific indications such as hypercalcaemia or Paget’s disease.
Adam Stewart
October 24, 2025 AT 10:28For anyone feeling overwhelmed by the table, just remember that each drug’s schedule matches its purpose. Didronel’s short bursts work well for intermittent conditions, while the yearly IV of zoledronate suits chronic bone loss.
Selena Justin
October 25, 2025 AT 17:10In accordance with current NHS prescribing policies, Didronel remains the first‑line therapy for Paget’s disease owing to its cost‑effectiveness and established efficacy. Nonetheless, clinicians must weigh individual patient tolerability, renal function, and fracture risk when selecting alternative agents.
Raghav Suri
October 26, 2025 AT 22:51Yo, the GI upset from etidronate is no joke – you’ll be tossing up after every dose if you’re not careful. Skip the drama and jump to a weekly alendronate if you can handle the esophageal precautions.
Freddy Torres
October 28, 2025 AT 05:33Larry nailed the technical side, but for real‑world patients the dosing hassle can be a deal‑breaker. Simpler regimens often improve compliance.
Andrew McKinnon
October 29, 2025 AT 12:15Sure, Xavier, let’s moralize over a cheap pill while ignoring that the real pain point is the ulcer‑inducing acid load. Your ‘ethical’ stance won’t heal a gut‑wrenching gastritis episode.
Dean Gill
October 30, 2025 AT 18:56Andrew, you’ve captured the frustration many patients feel when confronted with the archaic dosing schedule of Didronel.
First, the two‑week on/off cycle was designed at a time when monitoring tools were far less precise.
Second, the drug’s low binding affinity means that the bone turnover suppression is modest compared with later bisphosphonates.
Third, the gastrointestinal irritation stems from the acidic formulation required for oral absorption.
Fourth, patients with even mild esophageal reflux often experience burning sensations that deter adherence.
Fifth, the intermittent dosing does not provide the steady-state serum levels that weekly alendronate achieves.
Sixth, when you consider the overall fracture risk reduction, the numbers for Didronel hover around 10‑15%, whereas alendronate consistently shows 40‑45%.
Seventh, the cost advantage of Didronel is eroded by the need for repeated medical visits to monitor calcium and renal function.
Eighth, the alternative of a yearly zoledronic acid infusion eliminates daily pill fatigue entirely.
Ninth, for patients with chronic kidney disease, the low renal clearance of etidronate can actually be a safety benefit, but only under close supervision.
Tenth, the convenience factor of a subcutaneous denosumab injection every six months cannot be overstated for the elderly.
Eleventh, if you’re treating Paget’s disease specifically, the intermittent dosing aligns with the disease’s flare‑up pattern, making Didronel uniquely suitable.
Twelfth, however, you must remain vigilant for rare cases of osteomalacia with prolonged use, a side effect not seen with newer agents.
Thirteenth, patient education on taking the tablet with plenty of water and staying upright for 30 minutes mitigates some GI issues.
Fourteenth, in clinical practice, I’ve observed that when patients switch from Didronel to alendronate, their compliance improves dramatically.
Fifteenth, ultimately, the choice boils down to balancing cost, convenience, potency, and individual tolerability, and that decision should be made collaboratively with the patient.
Royberto Spencer
November 1, 2025 AT 01:38The bone, like a philosophy, holds the weight of our choices; selecting Didronel or its successors mirrors the eternal debate between frugality and ambition.