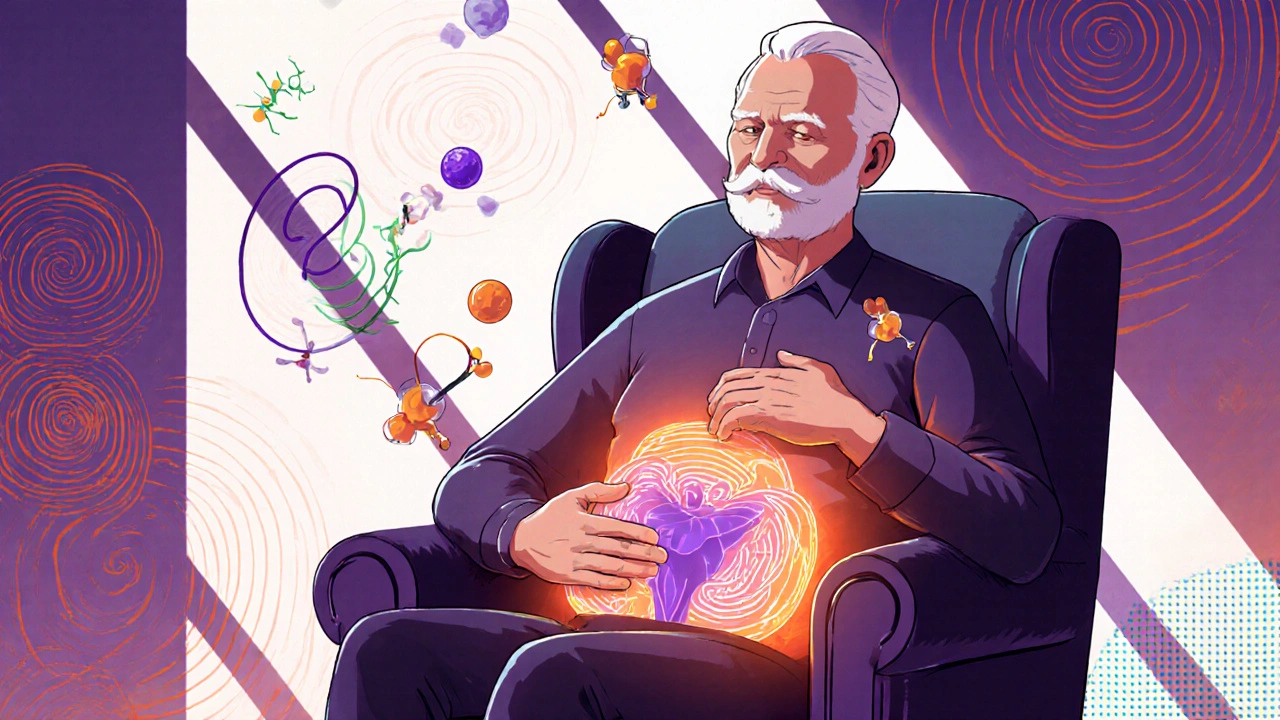
BPH (Benign Prostatic Hyperplasia): What It Is and How to Manage It
If you’ve heard the term BPH and wonder what it means, you’re not alone. BPH stands for benign prostatic hyperplasia, a non‑cancerous growth of the prostate gland that many men experience as they get older. The good news? It’s usually manageable with lifestyle tweaks, medication, or simple procedures.
The prostate sits just below the bladder and wraps around the urethra, the tube that carries urine out of the body. When the gland enlarges, it can squeeze the urethra and make it harder to empty the bladder completely. That’s why you might notice a weaker stream, frequent trips to the bathroom, or the feeling that you can’t finish urinating.
Spotting the Common Symptoms
Most men with BPH notice changes in their bathroom habits before anything else. Typical signs include:
- Needing to go more often, especially at night (nocturia)
- A sudden urge to urinate that’s hard to control
- Weak or interrupted urine flow
- Feeling like the bladder isn’t empty after you finish
If you have a few of these symptoms, it’s worth talking to a doctor. They can run a quick exam and maybe an ultrasound to see how big the prostate really is.
Simple Steps You Can Try First
Before diving into prescription drugs, many men find relief with everyday changes. Cutting back on caffeine and alcohol reduces bladder irritation. Staying hydrated—but not over‑hydrated—helps the bladder empty more efficiently. Try to schedule bathroom trips every 3–4 hours instead of waiting for an urgent need; this can train the bladder to hold more urine.
Pelvic floor exercises, also called Kegels, aren’t just for women. Strengthening those muscles can improve bladder control and reduce the feeling of incomplete emptying. A quick routine: squeeze the muscles you’d use to stop urinating, hold for five seconds, then relax. Do three sets of ten reps a day.
If lifestyle tweaks aren’t enough, doctors often start with medication. Alpha‑blockers like tamsulosin relax the muscle fibers around the prostate, making it easier to pee. For larger prostates, 5‑alpha‑reductase inhibitors such as finasteride can shrink the gland over several months. Your doctor will pick the right option based on prostate size and how severe your symptoms are.
When meds don’t fully help, minimally invasive procedures are available. Transurethral microwave therapy (TUMT) uses heat to reduce excess tissue, while laser vaporization removes small bits of the gland. Both are done in an outpatient setting, meaning you can go home the same day.
In rare cases where the prostate is very large or complications arise, surgeons might recommend a transurethral resection of the prostate (TURP). It’s a well‑established operation that removes a portion of the gland to relieve blockage.
Remember, BPH isn’t dangerous on its own, but untreated severe blockage can lead to urinary infections or kidney problems. Keeping an eye on symptoms and acting early makes a big difference.
Bottom line: if you notice any changes in how you pee, don’t brush them off. A quick chat with your GP can rule out other issues and set you on a path to smoother bathroom trips. With the right mix of habits, meds, or procedures, most men find solid relief and get back to their usual routine.
Avodart (dutasteride) shrinks an enlarged prostate by blocking DHT, improving urinary symptoms over time. Learn how it works, its side effects, how it compares to other treatments, and what to expect long-term.
Flomax is the go-to medication for many men dealing with the frustrating symptoms of benign prostatic hyperplasia (BPH). This article takes a practical, human-focused approach to explaining what Flomax is, how it works, the kind of results real guys can expect, and what to watch out for if you're thinking of starting it. You'll find the facts, relatable advice, and tips for making Flomax as effective and hassle-free as possible.